The leaflet is detailed below, or you can download the 'Radical Hysterectomy' leaflet in PDF.
Radical Hysterectomy
This leaflet has been written and produced for you, your partner and family to assist and support you, if you are considering or have been recommended to have this surgery. It is not intended to replace verbal information with your surgeon and specialist nurse. You can access other information via websites available – see end of leaflet.
Benefits and Reasons for having a Radical Hysterectomy
The aim of this surgery is to give the best possible outcome of your treatment management. You may want to know whether your treatment will work or whether you can stay well without treatment.
Your doctor will have explained that you have an early-stage cancer of the cervix. See leaflet ‘Cancer of the Cervix’.
Your partner and carer may also have concerns and questions about how they can help you, and how your condition and treatment will affect them.
Try to find out as much as you can about your treatment options and make a list of questions you may want to ask your doctor. (See information resources at back of leaflet).
Treatment Options & Choices
Your consultant with discuss with you the treatment options, and you may find the leaflet regarding understanding cancer of the cervix helpful.
What is a Radical Hysterectomy?
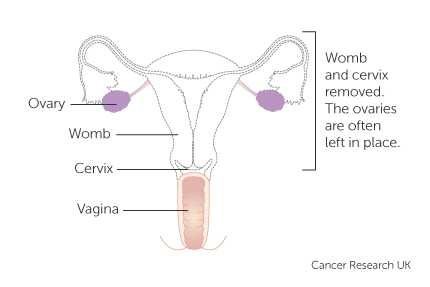
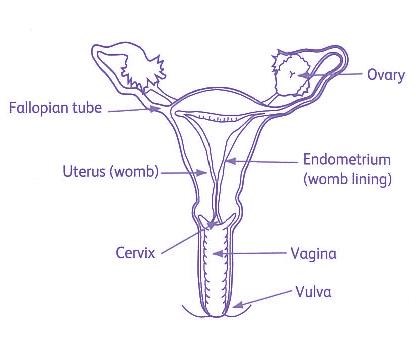
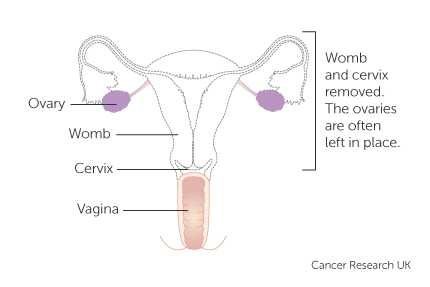
Hysterectomy is surgery to remove the Uterus (womb).
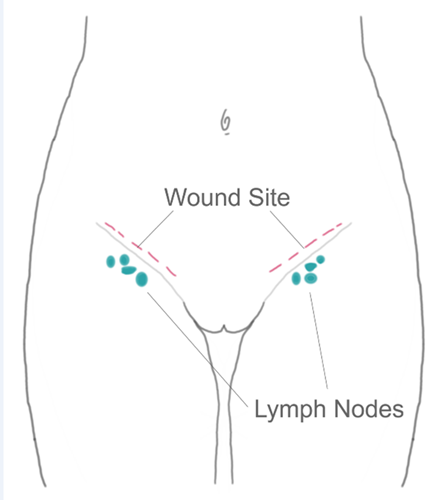
A radical hysterectomy means also removing a small part of the top of the vagina, some of the tissue either side of the neck of the womb, and lymph nodes. The operation takes 2 ½ - 3 ½ hours. Inpatient stay is approximately 3-4 days.
Your consultant will discuss with you whether to remove your ovaries or not. The incision (cut) in your abdomen (tummy) may be vertical (up & down) or transverse (across). Your consultant will discuss with you which is the most appropriate way in your circumstances.
What Happens Before the Operation?
You will attend Pre-operative Clinic the same day as Outpatients or shortly before the operation. During this visit the staff will discuss the type of operation you will be having and what to expect before and after. You will have the opportunity to ask any questions that you may have.
The pre-operative team will ask you to complete a health questionnaire and share with you written and verbal information about the Enhanced Recovery programme. It would also be helpful if you would make a list of all the medicines and drugs you are currently taking. A few tests may be performed such as blood pressure, urine test, blood tests and sometimes a chest x-ray or heart tracing. You may need to see an anaesthetist for assessment before your operation. The pre op staff will discuss with you blood thinning injections when you go home after your operation; there is a risk of blood clots after any surgery (and particularly after surgery for cancer), and the injections (for up to 4 weeks after the operation) will minimise this risk.
If you have any special requirements (physical/practical) for your admission such as a special diet or religious/cultural needs, please let the staff know during your visit so that all necessary arrangements can be made.
By attending the pre-operative clinic your future care can be jointly planned according to your individual needs, and all necessary steps taken to make your stay as comfortable as possible. If you feel you may need help following surgery, please discuss this with your GP or the nurse at the pre-operative clinic.
In Hospital – Before Your Operation
You will be admitted to the hospital on the day of your operation or the day before. As soon as you know you need an operation, try and get yourself into the best possible physical shape so that you can recover more quickly.
We would advise that you:
Stop smoking, eat a healthy diet and if able, take regular exercise. If possible, make plans with your family for while you are in hospital and arrange for some extra help for your first couple of weeks at home.
You will be admitted to the gynaecology admissions lounge where you will meet the gynaecology nursing team. The nurse will introduce herself and show you the ward layout.
Before you go into the operating theatre you will not be allowed to eat or drink for several hours before your operation. If you are in hospital the night before you will be asked to shower the morning of the operation, if coming in on the day please do this prior to admission.
There is usually an opportunity to meet the anaesthetist prior to surgery to discuss any concerns.
You may be given support stockings to wear during and after your surgery and you will also be prescribed an injection to reduce the risk of blood clots in the post-operative period. This is given as prescribed by the doctor. A member of the ward team will escort you to theatre and they will complete a checklist prior to you leaving the ward. The nurse will stay with you until the theatre reception staff takes over.
On arrival in theatre, you will meet the anaesthetist who will put you to sleep with an injection given via a small needle in the back of the hand. You will wake up in the recovery room after your surgery. Here you will remain for a short while for observation, before being brought back to your bed on the ward.
After Your Operation
You may feel some discomfort when you wake, and you will be given painkillers as required (see leaflet). You will have a drip in your arm and a catheter or small tube to drain urine from your bladder.
A Consultant will see you the day after surgery to review you and explain how the operation went and will advise you about resuming diet and fluids, they will also encourage you to get out of bed and slowly mobilise. This helps to prevent developing blood clots.
A slight discharge or some bleeding from the vagina is normal but if this becomes heavy you should tell your nurse straight away. You may get griping wind pains caused by bowel and stomach gas, which is normal, there are medicines which can help with this if required. You will be given a laxative to avoid constipation.
Your stitches are usually dissolvable so do not need removing. Occasionally the surgeons will use clips, and these will be removed by the district nurse or treatment room nurse and you will be informed when this will happen.
In some circumstances you may be discharged home with a catheter, this is to allow the bladder to recover following surgery. Before discharge, the ward staff will show you how to manage this when home, a plan will be made for you to return to the ward to have it removed.
Once home you will receive an enhanced recovery phone call from your Clinical Nurse Specialist to assess your progress.
Any tissue taken at the time of your operation will be sent for examination, this usually takes 4 -5 weeks and you will be informed of the results by your consultant via a face to face clinic appointment or telephone call. Following investigation, all tissue will be disposed of in accordance with health and safety. You may be asked if a fragment of any tissue removed to be kept as part of our ongoing commitment to research for future treatments into cancer. This would only be done with your consent.
Possible Complications
Although we try to make sure that any problems are kept to a minimum, no surgical operation can be guaranteed free of complications. The operation itself or the general anaesthetic may occasionally give rise to difficulties, which will make your stay in hospital longer or your recovery slower.
The risk of developing complications after surgery is increased in some patients. If you smoke, you are more at risk of a chest infection. If you are overweight or have diabetes you are more at risk of developing wound infection.
Frequency and Pain on Passing Urine
Occasionally, after a hysterectomy you may feel the need to pass urine more frequently. This is a result of slight bruising and swelling of the bladder. Pain relief such as paracetamol is recommended. It is also beneficial to exclude a urine infection if this persists.
Retention of Urine
We usually leave the catheter in the bladder for 5-7 days after the operation as there is an increased risk of retention after a radical hysterectomy than compared to a standard hysterectomy. We would usually aim to send you home with the catheter in place with a small leg bag under your trousers, with a plan to return for a Trial without Catheter (TWOC) a few days later. When you return and your catheter has been removed, you will have an ultrasound scan. This will look at whether you are emptying your bladder completely. It is important not to retain urine in your bladder, as it will become infected. If the scan shows you are retaining urine a catheter will be put back in and left for 1-2 weeks. This will allow your bladder time to go back to normal. Should you still be not emptying completely we will show you how to pass a small temporary catheter yourself. Again, this is only usually needed for a short period of time.
‘Wind Pain’ / Delayed Bowel Function
The operation can affect your bowel function and cause increased wind pain. This can cause pain in the abdomen, shoulder and back. Eating small quantities, especially of fruit and vegetables, and drinking plenty of fluid will help to re-establish your normal bowel movements. Painkillers and moving about will also ease the discomfort.
Occasionally the bowel can become sluggish and sometimes stop functioning as normal. This is known as an ileus. This can cause abdominal pain and distension, vomiting and constipation. If this happens you will have intravenous fluids (a drip) and not be allowed to eat until your symptoms settle, usually this takes a couple of days.
Constipation
It usually takes time for your bowels to return to their normal pattern; you will be offered laxatives to take after the operation to minimise any potential problems with bowel function.
Vaginal Bleeding / Discharge
Some women have a small bloodstained vaginal discharge after the operation.
Occasionally you can bleed quite heavily. This may be a sign that the wound inside your vagina is not healing, or that there is infection or a blood collection developing. If you are concerned about your bleeding, please tell the nurse looking after you and she will assess if it is normal.
If this becomes a heavy loss or an unpleasant smelling discharge when you go home, you are advised to contact your GP or the gynaecology ward.
Lymphoedema
Lymphoedema is swelling due to excess accumulation of fluid in the tissue. There is a risk of developing lymphoedema when pelvic nodes are removed. Secondary lymphoedema may develop in one or both legs. This will require specific ongoing management including the use of special hosiery, massage; skin care and exercises (see separate information leaflet). If you are at risk of developing lymphoedema, you will be monitored by a CNS within the team. You may also require a referral to a lymphoedema specialist for ongoing management, this would be made by your consultant.
Lymphocysts are a collection of lymphatic fluid which may occasionally form in the pelvis following pelvic node dissection. Only a small proportion of lymphocysts require treatment which is usually done by aspirating the cyst if symptoms develop.
Infection
With any invasive operation there is a risk of infection. Already mentioned are urine and vaginal infection. There is also a risk of developing a chest infection particularly if you have breathing related illnesses or you smoke. It is important to do deep breathing exercises after your operation. If necessary, you may be referred for physiotherapy, or need a course of antibiotics.
Another potential area of infection is the abdominal wound (cut on your abdomen) This can cause symptoms, such as redness around the wound; leakage from the wound or your temperature is raised. A member of the nursing staff will check your dressing each day. Please tell them if you are worried. It is also possible to develop a blood collection behind the wound; this would cause extreme bruising and tenderness.
Bleeding
It has already been mentioned that there can be bleeding from the vagina and the abdominal wound. Very occasionally patients bleed heavily during surgery, and it is necessary to have a blood transfusion. If you have any concerns regarding this, please speak with your Consultant or Specialist Nurse.
Damage to the Bowel or Bladder
Due to the nature of your surgery and the anatomy inside the pelvis there is a small risk of damage to either the bladder, the ureters (tubes to the kidney) or the bowel. The surgeon doing your operation would explain beforehand if you were at an increased risk.
If there are any problems during the operation these would be dealt with appropriately and you would be informed after your surgery.
Adhesions/Hernia
Almost all patients undergoing surgery on their abdomen will develop some adhesions. This is scar tissue which sticks together. They don’t usually cause symptoms and you are not aware of them. Rarely can they cause persistent pain or problems with bowel function. A hernia is a defect in the scar that can develop, occasionally this requires corrective surgery.
Developing a Clot
It is well recognised that having major surgery can cause patients to develop Deep Vein Thrombosis (blood clot in the leg) or Pulmonary Embolism (blood clot in the Lung), and this also is increased for gynaecological cancer surgery. As this is a known risk, all patients having major surgery are advised to wear anti embolism stockings until fully mobile, and blood thinning therapy (fragmin) is given each day for four weeks after your operation.
All the above are possible complication which will be discussed with you prior to signing your consent form. If you have any concerns, please speak to a member of the nursing team.
Returning To Work
Recovery time is variable for patients; a degree of tiredness is experienced for some time. Returning to work depends on the nature of your job. You must feel comfortable at work and be able to cope physically and emotionally. You will probably feel tired at first. You will need to refrain from work for at least 6-12 weeks. Your GP may advise you when to return, or your consultant when you see or speak with them during your follow up appointment. You will be discharged home from the ward with a 6 week sick note. Any subsequent notes required will be from your own G.P
Your Questions Answered
When Should I Stop Taking the Oral Contraceptive Pill?
You should stop taking it as soon as possible before your operation and use a barrier method instead. After the operation you will no longer be able to become pregnant.
How Does Having a Hysterectomy Bring About the Menopause?
The menopause happens when your ovaries stop producing eggs and therefore the hormones oestrogen and progestogen which control your monthly menstrual cycle are reduced.
You may already have experienced the menopause naturally. If your ovaries are removed during your laparotomy and you have not already gone through the menopause, then you will have your menopause straight away.
What Are the Symptoms of The Menopause?
Hot flushes and night sweats are the most common. These can be embarrassing, uncomfortable and can disturb your sleep. Dryness in the vagina can cause pain and discomfort when engaging in penetrative intercourse. Other problems are mood changes, tiredness, anxiety and loss of concentration. Hair and skin can become dry, and joints may be painful. In time, low oestrogen levels can cause osteoporosis (thinning bones) and heart disease.
How Can Hormone Replacement Therapy Help?
Hormone replacement therapy (HRT) relieves menopausal symptoms and can prevent osteoporosis. As the name suggests, this treatment replaces the oestrogen your ovaries no longer produce. There are many different types and strengths of HRT available. HRT can be given either as tablets to be taken every day or as skin patches which you change twice a week. Your doctor should be able to find a form of HRT to suit you.
When Should You Start HRT?
Your consultant will decide when and whether it is appropriate for you to start taking HRT.
Are There Any Side Effects With HRT?
Some women have nausea, breast tenderness or leg cramps at first, but this normally settles down quickly within the first three months. Others find that their skin becomes sensitive to skin patches. Occasionally headaches can become a problem. HRT does not cause you to put on weight.
What about Breast Cancer?
Breast cancer is a common disease in older women and 1 in 8 women in the UK will suffer from it. Studies show that taking HRT for up to 5 years does not appear to change the risk of getting the disease. Experts believe that if you have had your ovaries removed you can take HRT up to the time you would have had your menopause and then for an additional five years before there is any likelihood of change in risk.
There are also alternatives therapies/supplements to help with menopausal symptoms. These can be discussed with your nurse specialist.
Driving
Your movement and strength must be able to cope with an emergency stop before you return to driving. You should feel comfortable behind the wheel, with a seat belt over your abdomen. Recommended guidelines suggest 4-6 weeks. Or you could check with your insurance company.
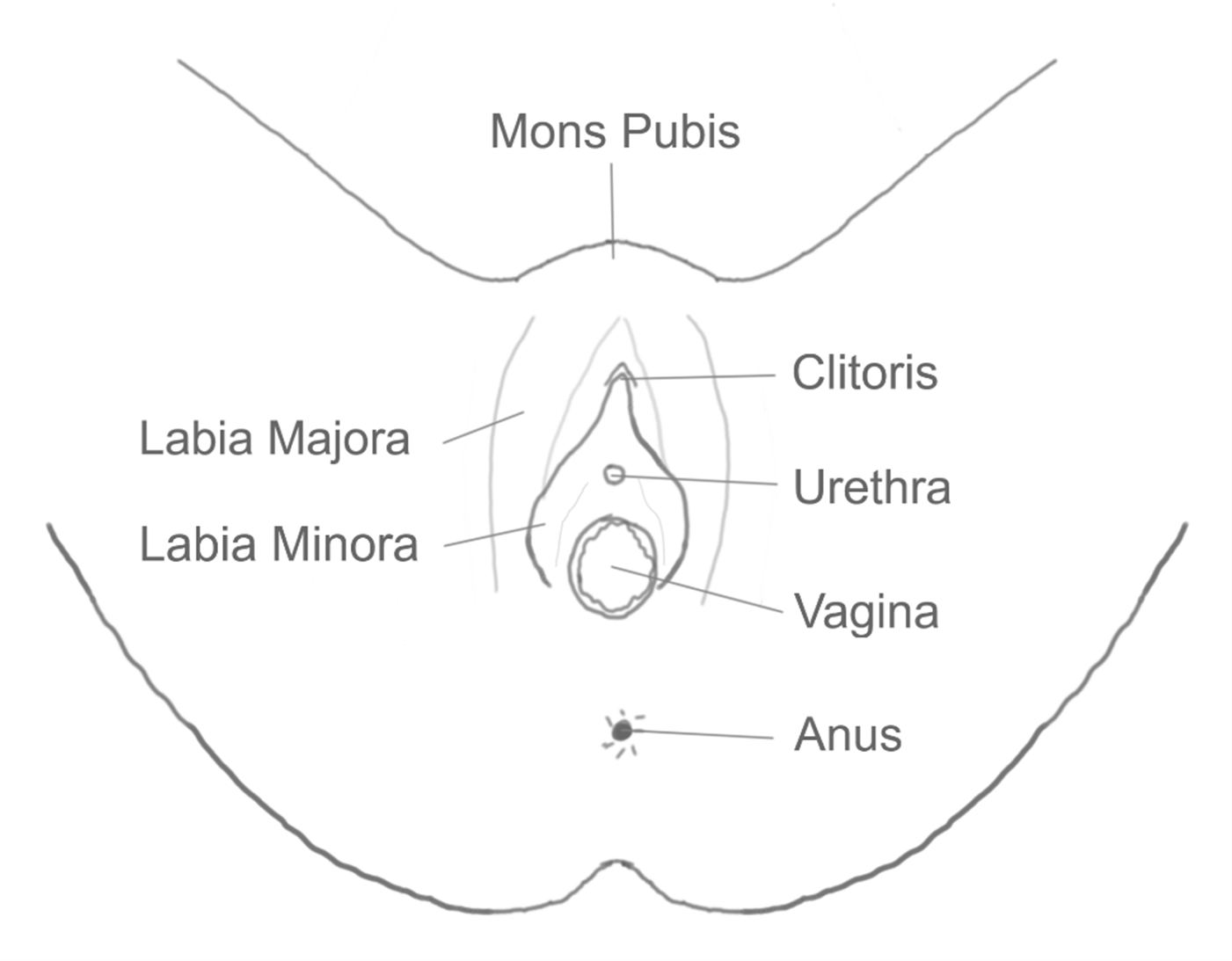
Sex
It is advisable to refrain from intercourse for at least 12 weeks after an open radical hysterectomy. This is to prevent infection and to reduce trauma. Resuming sexual intercourse will depend on the type and extent of surgery you have had and if you are worried about this then please speak to a member of staff before you are discharged.
Emotional Health
What Will I Feel Like?
After your operation, as after any big operation, you may feel low in mood, and tearful. This is a normal reaction, which the doctors and nurses understand. You may find it helps to talk with the staff caring for you, so don’t contain these feelings/emotions.
As time passes, you will begin to start feeling better, but you may still have ‘up’ days and ‘down’ days. It may take 6-12 months before you feel you have really adjusted physically and emotionally to what has happened. This is also normal. Some women find it helps to talk to their doctor, a specialist nurse or to one of the organisations listed at the back of this booklet. Please feel free to discuss your concerns.
Follow Up Appointment
You will be given a follow up appointment either in clinic or via telephone approximately 4-5 weeks after your operation; this will be sent out to you. At this appointment your doctor will have the report from the laboratory about the tissue from the operation. Depending on these results, you may need further treatment with radiotherapy (x-ray treatment) or internal radiotherapy, and or chemotherapy, administered intravenously. If this is recommended, your surgeon will discuss the treatment individually with you and you will also receive an appointment with your specialist nurse to discuss your treatment and any other support or information needs.
Will I Come Back for Check-Ups?
Yes, after your hysterectomy your consultant will ask you to attend hospital at regular intervals. You will be given an appointment for the outpatient clinic, initially every 4 months and over time the appointments will become less frequent. The follow up appointments will involve regular clinical assessment and vaginal examinations. (See - What to expect during your follow up care leaflet).
Your family doctor will have received details of your operation, so if you feel that things are not gradually returning to normal when you are at home, you might like to discuss this with him/her. Well-meaning friends, relatives and even other patients can give inaccurate and sometimes alarming information. Although many women are sometimes embarrassed to talk about themselves after this operation, it may be helpful for you to share your concerns with your family doctor or practice nurse. If you are still worried you may wish to contact the hospital.
Equal Opportunities
The hospital is committed to promoting an environment, which provides equal opportunities for all patients, visitors and staff. If you have any special requirements such as dietary needs, interpreter services, disability needs or a preference for a female doctor do not hesitate to discuss this with a member of staff who will try to help you.
Where Can I Get Help?
If you have queries or problems regarding your illness or operation, or experience any unexpected problems, please contact:
- Your hospital doctor (Consultant)
- or one of their team
- or specialist nurse
- or your family doctor/ practice nurse / community nurse
Both National and local leaflets/information are available on all aspects of your recovery. Please ask your nurse specialist for further links to this information.
Further Help
The staff on the ward are always available to discuss these and any other issues with you fully, please do not hesitate to ask.
A cancer information service is also provided by these organisations:
Tel: 01793 302005
www.communigate.co.uk/wilts/gynae
www.jotrust.org.uk
- The Daisy Network (Menopause issues)
PO Box 183
Rossendale
Lancs
BB4 6WZ
www.daisynetwortk.org.uk
Cancer Support Line: 0808 808 0000
www.macmillan.org.uk
www.menopausematters.co.uk
- Lymphoedema Support Network
Tel: 020 7351 4480
www.lymphoedema.org.lsn
References:
Gynaecology
Shaw, Southler & Stanton
Published by Churchill Livingstone
Natural Alternatives to HRT
Marilyn Glenville.
Published by Kyle Cathie Ltd, 1997.
ISBN 1-8-5626-254-5
Hysterectomy –
The emotional aspects,
Published by Dennerstein, Wood & Burrows
Hysterectomy – What it is and how to cope with it successfully
Suzie Hayman – Sheldon Press,
ISBN -0-859-69-870X,
Biddles Press Ltd.
www.biddles.co.uk
Our Bodies Ourselves
Jill Rakusen & Angela Phillips
Published by Penguin
A Woman’s Guide to Hysterectomy –
Expectations Options
Published by Celestial Arts,
ISBN 1-58761-105-8
The Menopause
Rosetta Reitta
Published by Penguin