Each of the Maternity leaflets are detailed below, select the heading of the one you would like to view and the content will expand with an option for you to download the PDF version.
Leaflets can be made available in difference formats on request, to view in a different language select the language change in the bottom left of the screen.
We would really like some feedback on our e-leaflets. If you could take a couple of minutes to complete our short feedback form by clicking here that would be much appreciated.
If you would like to make any suggestions or comments about the content of this leaflet, then please contact the Patient Experience Team on 0151 702 4353 or by email at Pals@lwh.nhs.uk.
Changing language options online using Google Translate
Please note that Google Translate is the tool that is used to translate information on our website to other languages. Google Translate is a global tool that is not under Liverpool Women’s control. Therefore whilst you may use Google Translate for useful simple translations, it should not be relied upon as a substitute for official translation services that are provided by the Trust. Please take particular notice of this when you are using the translation feature for patient information that contains detailed clinical information. Speak to a member of staff when you visit the Trust if you require any translation support.
-
Postnatal Pain Relief Video
-
Post-Natal Pain Relief
The leaflet is detailed below, or you can download the 'Post-Natal Pain Relief' leaflet in PDF.
Why have I been asked to read this leaflet?
You have been given this leaflet to read alongside the pain relief you will take home after the birth of your baby. This leaflet is to help you understand the pain relief options that are available to you, how to take them and the common side effects. If you have any further questions or concerns, please do not hesitate to ask you midwife or doctor.
What tablets will I be given?
We aim to give you a range of medications to help with your pain. Each of these medications are safe to take together and work in different ways so they complement each other to give you the best pain relief.
- Paracetamol
This is the same medication that you can buy over the counter. You can take two tablets up to four times a day. Each tablet is 500mg so this means you are taking 1g each dose. You should not take more than 4g (8 tablets) in 24 hours. Make sure you do not take any other medication that contains Paracetamol, such as cold and flu medications alongside your Paracetamol. If you do take more than 4g in 24 hours you should seek medical help via 111.
It is considered safe for breastfeeding.
More information below in the section: Are these tablets safe for breastfeeding?
- Naproxen
This is similar to Ibuprofen and is known as a Non-Steroidal Anti-inflammatory or NSAID for short. You can take 500mg twice a day. We advise you to take Naproxen with food as it can cause stomach upset. It is considered safe for breastfeeding.
More information below in the section: Are these tablets safe for breastfeeding?
There are some occasions when we would not advise NSAIDs. These include
- Blood pressure problems such as pre-eclampsia
- Very heavy bleeding
- Kidney problems
- Low platelets
- Asthma
- Stomach ulcers
Dihydrocodeine
This is a Codeine-like pain killer (a bit like Morphine) which is commonly effective for moderate to severe pain. You can take one (30mg tablet) every six hours. This means a maximum of 4 tablets in 24 hours. It is best taken as and when pain is most severe, for example in the early days after giving birth or after surgery. It can work best when taken before performing tasks which result in excess pain. It is considered safe for breastfeeding. More information below in the section: Are these tablets safe for breastfeeding?
It is strongly advised that this drug is not given to anyone else other than who it has been prescribed for. Any excess tablets left over when you have recovered should be returned to a local pharmacy/ hospital pharmacy or GP surgery for safe disposal.
A reliance on taking Dihydrocodeine can become a problem with prolonged use, which is why limiting it for severe pain episodes will give you better control of your pain. We would not expect you to need strong pain relief like Dihydrocodeine for longer than 2 weeks. If you are still struggling please contact us at the Maternity Assessment Unit or through your GP.
It is rare, but people can develop an addiction to pain killers such as Dihydrocodeine with prolonged use is even though the pain killer action is no longer offering them pain relief qualities. Continued use of pain killers after 90 days is called chronic pain. If you have any worries about this please speak to us here at the women’s or speak to your GP.
How can I get the best out of my pain relief?
Take Paracetamol and/ or Naproxen at REGULAR intervals in the first two or three days after leaving hospital (they can be administered safely together or with time gaps). Taking pain medication regularly like this helps you to keep on top of the pain as it gives you a constant background level of pain relief.
In combination with these regular doses, you can take Dihydrocodiene AS AND WHEN the pain is at its worst or when you know you are going to be particularly active such as before a shower, or a walk. You can take one 30mg tablet every six hours. This means a maximum of 4 tablets in 24 hours.
At the end of this leaflet is a table that may help you to keep track of what you have taken and when. Having a newborn baby can make it difficult to keep track of your medications.
You will become good at balancing the need for pain relief medication, soon not needing any. You'd probably expect this to be within a week or two.
What are the common side effects of these tablets?
Most women will not have any side effects with Paracetamol when it is taken in the correct dosage. Naproxen can cause acid reflux and stomach ulcers. This is why we always advise you take it with food. If you develop problems with stomach pain we advise you to stop taking this medication.
Dihydrocodeine can case constipation. This can be avoided by making sure you drink plenty of fluids and have a high fibre diet. It may be that you need laxatives to help avoid this. Over the counter medicines are safe to take but if you are breastfeeding please check with your doctor or pharmacist what is the best option.
Dihydrocodeine when taken at rest may make you drowsy, and not make the best use of this strong drug. It affects some people more than others in this way.
Special attention must be given to taking Dihydrocodeine if planning on driving as it may lead to an increase in chances of drug-related road accidents and invalidate your vehicle insurance.
Are these tablets safe for breastfeeding?
We have chosen these medicines so that they are safe for mums no matter how they choose to feed their baby. Some manufacturers advise to avoid Naproxen with breastfeeding. It is common for manufacturers to advise caution for their medications in pregnancy and breastfeeding due to licensing of the product rather than the effects on mum or baby. We are happy to recommend Naproxen for breastfeeding mums as the amount found in breast milk is very small.
More information can be found on the breastfeeding and medication website. Accessible at https://breastfeeding-and-medication.co.uk/ or via their information leaflet which can be found at https://breastfeeding-and-medication.co.uk/fact-sheet/naproxen-and-breastfeeding
Will I be given tablets to take home?
Yes. We will be giving you a week long supply of your tablets to take home. We would advise you to take the tablets regularly at first and then reduce them as you feel you need less. It is best to taken the pain relief regularly when you first need it as it works better this way. You may find that as you start to do more activity when you are at home compared to being in hospital you have an increase in your pain. This can be normal and we would suggest taking your medications more regularly if you find this happening.
What should I do if I am still in pain?
As we all have different birth experiences there may be some women who need more pain relief. If you are still in hospital please alert your midwife or doctor and the will assess you and make a plan with you for more pain relief.
If you are at home your community midwife will be visiting you so please let them know you need more pain relief. If the midwife is not visiting you that day or you cannot wait please call the Maternity assessment unit to speak to a midwife for advice.
Maternity Assessment Unit 0151 702 4164
-
Caring for my Caesarean Section Wound after Delivery
The leaflet is detailed below, or you can download the 'Caring for my Caesarean Section Wound after Delivery' leaflet in PDF.
Foreword
This booklet is intended for patients who have already undergone a caesarean section, the information provided is applicable for after your surgery.
If you are looking for information regarding what to do before your surgery please visit our website and look under ‘patient leaflets’ and you will find all of the pre-operative information.
What is a Caesarean Section?
A caesarean section, or C-section, is an operation to deliver your baby through an incision made in your stomach and womb, usually positioned just below your bikini line. This is usually around 15-20cm in length.
Around one in four pregnancies result in a caesarean section birth.
Why do people have Caesarean Sections?
Women have C-sections for many reasons, either by choice or for complications during vaginal delivery. For whatever reason, your recovery should be the same.
How long until I recover?
Generally, it takes around six weeks to recover from a c-section however this will depend upon your individual situation, if your surgery had complications, or if you have other young children at home meaning you are resting less, you may feel you need more time.
Gentle exercise such as walking will help recovery but avoid anything strenuous and ask for help when lifting heavy things. This includes, lifting prams and car seats.
Looking after your C-section wound
Your midwife will visit you at home 5 days after your delivery where baby checks will be completed and the dressing to your wound will be removed UNLESS you have a PICO dressing (PICO dressings are explained in detail later on in this leaflet).
Check with your midwife before you leave the hospital if you have absorbable stitches or if your stitches require removal. If your stitches require removal please make an appointment with your practice nurse for this to be completed or your community midwife will remove them for you.
Once your dressing is removed, clean and dry your wound thoroughly every day with plain water (no soaps or oils), do not have a bath i.e. submerge your wound fully in water for two weeks, you may shower and allow the water to run on your wound, do not scrub or massage.
After having a shower pat dry your wound with a clean towel, separate from the one you have used to dry your body
Do not touch your wound unless it is necessary and you have thoroughly washed your hands.
It’s really important that you look out for any redness, swelling, excess bruising, weeping, smell, pus or opening of the wound; the sutures should have dissolved by 3-4 weeks. Speak to your GP if you feel unwell, have more pain or a temperature.
Try to avoid wearing underwear where the banding has direct contact with the wound. Wearing loose fitting or high waist underwear is better.
Between 5-6 weeks your wound should have healed into a scar, this will be pink/red at first and then gradually fade. You may find that you have an altered sensation in the close proximity of the wound however this will come back eventually.
Smoking
If you smoke, you should make every attempt to give up before your surgery. Smoking significantly reduces the amount of oxygen that can be distributed to your tissues; this in turn slows down wound healing. You can receive help and support to give up smoking from your GP or practice nurse.
Diet
Your body needs energy and the right nutrients to encourage good healing. A healthy balanced diet with lots of protein will help; you don’t usually need to take supplements. Ensure you are thoroughly hydrated as this will also help healing.
Weight
Unfortunately those whom have a high body mass index (BMI) are more likely to have a wound infection or experience healing problems with wounds.
Diabetes
If you have diabetes, it is important that your blood sugar is well controlled – having high blood sugar can increase the chances of having a wound infection or slowing down the healing process.
PICO Dressing
Your consultant surgeon decides if you are to have a PICO dressing, they will select this dressing if you are at risk of a wound infection due to a higher BMI or because of a long term condition such as diabetes.
A PICO dressing is a negative pressure device, which has a life of one week and then discarded.
Using a negative pressure dressing places the two sides of the wound under pressure, decreasing tension, removes any moisture, increases blood flow to the wound site and overall helps to prevent infection.
Your midwife will remove PICO on day seven after your delivery. Please note: the PICO box contains removable AA batteries; please be aware of this if children are around.
The PICO box is NOT waterproof, although the dressing itself is. If you have a shower unscrew the box from the dressing and put in a safe place; after showering reconnect and press the orange play button.
Troubleshooting with PICO
You should not have to do anything apart from unscrewing the box when you shower, however it is important that you keep an eye on the box to make sure you are receiving the negative therapy. It will be flashing green on the left hand side if it is.

If PICO is flashing for a leak: Lay yourself as flat as possible and smooth the edges of the dressing down and press the orange button again. Repeat the process until a seal is obtained and the OK light is flashing green.
If PICO’s full indicator is flashing: Observe the dressing, if there is a lot of staining on your dressing it will need to be changed; let your midwife know or call us and the dressing will be changed. If there isn’t a lot of staining and its flashing this, press the orange button and it should reset.
If PICO is flashing for the battery: The batteries are designed to last for 1 week, PICO should not flash for this reason unless it is day 7.
If you continue to experience problems with PICO ask your midwife or call us on the hospital switchboard and ask for the tissue viability nurse or MAU department.
Hospital switchboard: 0151 708 9988
Pain after Caesarean Section
You will feel sore for a few weeks; you may need pain relief for one week to ten days after your delivery. Discuss with your midwife or doctor before taking any pain relief as some strong pain killers are not safe to take whilst breastfeeding.
Mobilisation techniques for getting in and out of bed may also help with the pain. Try rolling onto your side, dropping both legs over the side of the bed and pushing yourself sideways into a sitting position. Then complete the opposite for getting into bed.
Preventing blood clots
Keeping as active as possible and keeping hydrated will help to lower your risk of blood clots, you may have injections to inject yourself every day if you are particularly at risk.
Call 111, tell your GP, health visitor or midwife straight away if you have signs of a blood clot, these are: sudden redness, swelling or pain in your legs/calf area, shortness of breath, or chest pain.
Where can I get further information about infections in hospital?
The Public Health England website www.hpa.org.uk has a section on surgical wound infections which includes the latest report. More information about surgical wound infections can be found in the guideline on the Prevention and Treatment of Surgical Site Infection published by the National Institute for health and Clinical Excellence in 2008, and can be found online at www.nice.org.uk.
If you have concerns regarding infection or infection prevention, please speak to the nurse looking after you. You can also discuss your concerns with a matron or a member of the Infection Prevention and Control Team on 0151 702 4014.
-
ECV - Liverpool Women's External Cephalic Version
Are you booked for a ECV at Liverpool Women's? Are you unsure what to expect?
Here we have two of our specialist Obstetric Consultants explain the ECV procedure and demonstrate a successful attempt to turn a baby. Click the link to watch the full video
-
Why Have I Been Referred To The Fetal Medicine Unit?
The leaflet is detailed below, or you can download 'Why Have I Been Referred To The Fetal Medicine Unit?' leaflet in PDF
Your sonographer suspects or has found an issue with your scan today. This could be related to your baby, your placenta or your cervix. The sonographer will explain to you the reasons for their concerns but the exact nature of the issue may not be clear at this stage. You will be offered an appointment to see a specialist consultant in the Fetal Medicine Unit at the Liverpool Women’s Hospital. At this appointment they will assess the issue further via a specialist scan.
What is the Fetal Medicine Unit?
Most pregnancies progress without any complications. However, sometimes a mother or her unborn baby needs extra care from our highly experienced Fetal Medicine team - made up of specialists including fetal consultants, midwives and healthcare assistants. As a specialist unit within Liverpool Women’s, we receive many referrals from health professionals throughout the North West and further afield.
When Will I Be Seen?
We aim to offer you an appointment within 3-5 working days from your ultrasound scan in our Fetal Medicine Unit. However, if your baby is suspected as having a problem needing specific multidisciplinary input you may wait a little longer in order to see the appropriate professionals.
What Happens Next?
We know this is a worrying time for you and your family. We are aware that it is very stressful waiting for a follow up scan to clarify the findings. You will be contacted by a Fetal Medicine Midwife by telephone or post to inform you of the date of your appointment as soon as possible.
Who Can I Contact For Further Information & Support?
- Fetal Medicine Unit 0151 702 4072 9-5pm Monday to Friday
- Antenatal Results & Choices (ARC) – a national charity helping parents and healthcare professionals through antenatal screening and its consequences - 020 7713 7356 or use this web address: https://www.arc-uk.org
-
Skin to Skin Contact with your Baby
The leaflet is detailed below, or you can download 'Skin to Skin Contact with your Baby' leaflet in PDF.
Skin to skin contact is beneficial for both you and your baby. Your midwife will offer skin to skin contact to you at delivery.
Why Skin Contact Is Important
- Keeps baby warm
- Calms you and your baby
- Your baby’s heart rate and breathing will be better controlled
- Encourages bonding between you and your baby
- Regular periods of skin contact in the early month increases a baby’s brain development
- Skin contact and early feeding promotes successful breastfeeding
Weighing Your Baby
Your midwife will either weigh your baby soon after delivery and then you can have skin contact or you can have skin contact first and then have the baby weighed later.
How to Do Skin Contact
After birth your baby will be gently dried and placed on your chest in an upright position, with their chest to your chest. A blanket will be placed over your baby but not covering the baby’s head.
Whilst baby is in skin contact make sure you can see your baby’s face and can hold your baby safely. It is advisable that your birth partner stays with you in the room after delivery while you are having skin contact with your baby.
Skin to skin contact should continue uninterrupted for as long as possible immediately after delivery and continue long enough for the baby to show signs of being ready to feed (this can take up to an hour or more). You can of course choose to end this contact whenever you wish.
Make the most of this special time immediately after the birth of your new baby. At no other time will you or your baby have such high levels of hormones to encourage bonding. Your baby will, if left uninterrupted in a quiet and unhurried environment go through a pattern of behaviour to show that he/she is ready to feed. At this point you will be offered help to feed your baby.
If you require a caesarean section to deliver your baby, we will ensure that you will receive skin to skin contact as soon as possible after your operation.
All mums regardless of type of birth can be transferred to the postnatal ward in skin contact if they wish.
Points to Remember
In the early days skin to skin contact will be of great benefit in encouraging your baby to feed and for you to get to know your baby. Skin to skin contact will help to keep your baby warm so do not worry about your baby getting cold.
Skin to skin contact is useful at any time in a baby’s first year of life e.g. if your baby is very unsettled. The close contact and warmth from your body along with your regular heart rate and breathing will comfort and calm your baby. Partners can also have skin contact to help settle and get to know their baby.
Babies Admitted To Neonatal Unit
Sometimes it may not be possible to have skin to skin contact with your baby straight away, for example if your baby is unwell or very premature. However, skin to skin contact can be introduced gradually as your baby gets better. There are huge benefits of skin to skin contact for premature babies and we actively encourage this.
For more information ask your midwife
-
Information for Pregnant Women with a raised BMI
The leaflet is detailed below, or you can download 'Information for Pregnant Women with a raised BMI' leaflet in PDF.
Women who are overweight are known to be at increased risk of developing problems during pregnancy, delivery and after giving birth.
Rather than just using weight to assess who is at risk, we use BMI (Body Mass Index), which is takes into account people’s weight and height. It is a nationally recommended way of assessing health issues associated with weight. Internationally, a figure of 19-25 is classified as normal; 25-30 is overweight,
30-40 is obese and over 40 is very obese.
Pregnant women with a BMI of 30 or more are more likely to have:
- Diabetes in pregnancy
- High blood pressure problems
- Difficulties with assessing the growth and wellbeing of the baby
- Caesarean sections
- Complications associated with caesareans or forceps deliveries
- A higher risk of developing clots in the legs or lungs
- Anaesthetic complications
Antenatal Care
Women with a BMI of 35 or over will be referred for consultant-led care and will be offered a glucose tolerance test (GTT) around 28 weeks of pregnancy to assess their body’s ability to handle sugars and detect any tendency towards diabetes during pregnancy.
Women with a BMI of 40 or more will also be offered this test and will be referred to consultant led care and an antenatal clinic with a specialist midwife. Ideally women with a BMI of 30 or more should have taken folic acid 5mg up until 12 weeks. Some women may also be prescribed a vitamin D supplement and aspirin during pregnancy.
Scans
Scanning the unborn baby of a woman with a high BMI is technically more difficult as much of the power of the ultrasound waves is absorbed by the mother’s tissues. Therefore the images obtained may not be as accurate as those normally obtained. This may mean a reduced ability to detect problems, for instance at the 20 week anomaly scan. Further scans for growth may be arranged by the consultant or midwife, if they are concerned about the growth of the baby as pregnancy progresses. A scan may also be performed at
36 weeks of pregnancy to confirm which way the baby is lying and make a plan for the birth.
Labour and Birth
If you have a raised BMI 35 and above, you may not be suitable for the midwifery led unit and may be advised to give birth on the delivery suite, but this can be discussed with your midwife or doctor. If your BMI is greater than 40, you will be advised to give birth in the delivery suite.
Pain Relief in Labour
There are a number of options available to you for pain relief during labour. These include Entonox (‘gas and air’), water (if you are on the Midwife led unit), diamorphine and an epidural. Being overweight can mean there is an increased risk of complications if you have an anaesthetic during labour and birth (epidural or spinal). Therefore, if your BMI is 40 or more, an appointment will be made for you to see an anaesthetist during your pregnancy, who will discuss this with you and make a plan for when you are in labour, should you wish to have an epidural.
Postnatal Care
If you have a caesarean section, recovery following the operation may be slower. You will be given antibiotics when you are in theatre to help prevent any infections. You are also encouraged to get out of bed as soon as possible to help reduce the risk of blood clots developing in your legs or lungs and you may also need to have a daily injection to ‘thin’ your blood to help prevent this. These injections will be for at least seven days after you have had your baby.
Feeding Your Baby
Breastfeeding gives your baby all the nutrients it need for the first 6 months. Breastfeeding is recommended as the best way to feed your baby. Support to start and continue breastfeeding is available when you are in the hospital after having your baby and when you go home.
Weight Loss after Having Your Baby
After having your baby it is important that you try to lose weight, in order to reduce your BMI. There are a number of weight management services available in your local area that can assist with weight loss. Make an appointment to see your GP, who will be able to advise you on weight management and refer you to services in your local area.
Finally……
Liverpool Women’s Hospital is at the forefront of research into the way that a woman’s weight affects her pregnancy. If you attend the specialist antenatal clinic, you may be invited to take part in some research studies that have been set up to develop our understanding of this common problem. Please do not hesitate to ask if you have any particular concerns or for any further explanations with regards to your care.
For more information ring: 0151 702 1126
www.nhs.uk/start4life/Pages/Welcome-to-Start4Life
www.eatwell.gov.uk
-
Iron Sources
The leaflet is detailed below, or you can download 'Iron Sources' leaflet in PDF.
Teenage girls and women under 50 years old should have 14.8mg of iron per day
Iron Sources
An average serving is roughly the size of a pack of cards.
Roast Beef contains
2.3mg
Per average serving
Bran Flakes contains
6mg
Per bowl
Baked Beans contains
2.8mg
Per half tin
Boiled eggs contain
1mg
Per small egg
Sardines contain
1.5mg
Per 50g serving
Figs contain
3.4mg
Per 4 figs
Green Veg contains
1.96mg
Per average serving
Avoid drinking tea and coffee with meals. Both drinks contain chemicals that reduce the amount of iron you absorb from your food.
Drink them an hour before you eat or two hours afterwards. So, it’s better to have a glass of orange juice with your bowl of cereal in the morning than a cup of tea.
-
Promoting Breastfeeding within Liverpool Women’s
The leaflet is detailed below, or you can download 'Promoting Breastfeeding within Liverpool Women’s' leaflet in PDF.
Breast milk gives babies all the nutrients they need for the first six months of life, helping to protect them from infection and diseases, and reduce the rate of asthma and obesity.
For mothers, it reduces the chances of getting certain diseases, such as ovarian and breast cancer, and also protects against developing weaker bones in later life.
How you feed your baby is a very personal decision and midwives will support women and families in their choices. If the decision is not to breastfeed, a supply of milk will need to be brought in to the hospital. This should be the ready prepared variety in cartons and not the powdered formula which needs preparation. Bottles and teats will still be provided.
Therefore we do not supply formula milk for mothers who choose to artificially feed their babies.
We will also provide information and a demonstration on how to prepare formula feeds and sterilise bottles, if this is the chosen method of feeding.
If there are any questions or concerns, then women should not hesitate to contact their midwife for advice or the ward manger on the maternity ward on: 0151 708 9988 extension 1331.
-
Pre-eclampsia - Things You Should Know About Pre-Eclampsia
The leaflet is detailed below, or you can download 'Pre-eclampsia' leaflet in PDF.
What Is It?
An illness which occurs only in pregnancy and can affect both a mother and her unborn baby. Most cases are mild, but there is a severe form which can be dangerous. Among the most serious complications are convulsions known as ‘eclampsia’ – hence the term pre-eclampsia.
Who Gets It?
About one pregnant woman in every 10. Most at risk women are first-time mothers; the over 40s; those with a BMI over 35; women with a family history of preeclampsia: where it is ten years or more since a last baby; those suffering from high blood pressure, diabetes or kidney disease; those carrying more than one baby and those who have had it before.
What Causes It?
A problem in the placenta which restricts the flow of blood to the baby. This problem develops in early pregnancy but doesn’t cause illness until much later – usually the last few weeks.
What Are The Signs?
High blood pressure, protein in the urine in the mother, and sometimes, poor growth in the baby – all of which should be detected by routine ante-natal checks.
How Is It Treated?
Women with pre-eclampsia are monitored carefully – usually hospital or a day ward – and may be given drugs to control blood pressure.
-
Having Anorectal Tests
The leaflet is detailed below, or you can download the 'Having Anorectal Tests' leaflet in PDF.
What Are These Tests For?
Anorectal tests are offered here at LWH as part of the routine follow up for Obstetric Anal Sphincter Injury (OASI). This is due to the fact that women that have had these types of tears are more likely to experience difficulty controlling the muscles around the back passage. This may be because the anal sphincter muscles have become weak or damaged. This may cause you to have urgency or leakage of stools (faecal incontinence), or you may have trouble with controlling wind (flatal incontinence). Anorectal studies enable us to gain a better understanding about how your tear has healed and how your back passage is functioning.
What Are Anorectal Tests?
There are two different tests that provide information about the sphincter muscles and how they are working. These are:-
- Endo-anal ultrasound
This uses ultrasound to provide an image of the anal sphincter muscles to see if there are any defects present. An ultrasound probe is passed into the back passage and gently withdrawn to allow different views of the anal sphincter to be seen.
- Anorectal manometry
This provides information on the strength of the anal sphincter muscles and its ability to relax and contract. A small flexible tube is passed through the back passage into the rectum. On the end of this tube is a transducer that records the pressure inside. During this test the tube is slowly pulled outwards from the back passage to the edge of the anal sphincter. You will be asked to squeeze the muscles in your back passage several times during this test, in the same way you do your pelvic floor exercises.
The appointment for these tests is 45 minutes; however the actual testing takes no more than 10 minutes to perform.
Where Will These Tests Take Place And Who Does Them?
These tests take place in the Urogynaecology Department and are done by a Doctor or the Urogynaecology Link Midwife. Sometimes there may be a member of staff who is training observing the tests, however you will be informed of this and you can decline to have them present.
Will I Need Any Special Medication And Will I Be Able To Take My Usual Medication?
The tests will be more comfortable for you if you have been able to empty your bowel prior to the test. No specific medications to empty the bowel, such as laxatives, are required for the tests. You should continue with any other medication that your doctor has prescribed for you.
Questionnaire
You will be asked to complete an online questionnaire (ePAQ) as part of your care. This is a self-assessment questionnaire which gives us more information about your symptoms. It is confidential.
What Will Happen When I Arrive At The Urogynaecology Department?
You will need to use the self-check-in machines located in the main reception of the hospital or the gynaecology outpatient main reception. This then informs you of the waiting area you should head to and lets the staff know you are in attendance. You will then be called through by the Midwife when she is ready.
What Will Happen During The Tests?
- The Midwife will take you into the room where you will be asked questions similar to those you were asked when you attended for your 6-8 week follow up, regarding any bladder or bowel symptoms you may have experienced.
- Each test will be explained to you and you will have the opportunity to ask any questions.
- You will then be asked to change into a hospital gown and taken to the treatment room for the examination to be performed.
- You will then lie on your left side on an examination couch.
- You will have a sheet to put over you.
- When all the tests are complete you will be able to get dressed.
- Occasionally patients feel the need to go to the toilet immediately following the test. This is due to the stimulation of the rectum and is quite normal so no need to worry.
Are The Tests Painful?
You may have a feeling of pressure during the tests but they should not cause any pain. You can ask the person performing the tests to stop at any point if you are not comfortable.
Should I Attend If I Am On A Period?
Yes. Being on a period does not affect the results of the tests.
When Will I Get The Results Of My Test?
The Urogynaecology Consultant will see you after the examination and discuss the results with you. You will also be advised regarding the mode of delivery we would recommend for future pregnancies, depending on the results of the tests and taking into consideration any symptoms you may have.
If you have any questions about these tests you can contact the Urogynaecology Link Midwife on 0151 702 4321 for advice.
If you need to rearrange your appointment please telephone the Patient Appointment Centre on 0151 702 4328 (option 2) as early as possible.
Some useful resources:
-
Intramuscular progesterone for women attending the preterm birth prevention clinic
The leaflet is detailed below, or you can download 'Intramuscular progesterone for women attending the preterm birth prevention clinic' leaflet in PDF.
What is Progesterone?
Progesterone is a natural hormone. It is produced by your body in pregnancy.
What is preterm birth?
This refers to birth less than 37 weeks of pregnancy. Babies that are born preterm have an increased risk of health problems. The team in the preterm birth prevention clinic aim to work with families to reduce their risk of preterm birth.
Why is it important for women attending the preterm birth prevention clinic?
Research has shown that extra progesterone can help you have a full length pregnancy.
You have been identified as someone who has a higher risk of preterm birth. This is because in a previous pregnancy your baby was born early, or your waters broke early. A medication to prevent preterm birth could be especially helpful in your pregnancy.
What does the research say I should do?
If you are pregnant with one baby-
- Use progesterone from 16 to 36 weeks of pregnancy
- Progesterone is given as an injection into a muscle. This is normally a muscle in your bottom.
- The injection is given weekly
How much will this help?
Your doctor will be able to discuss this more fully with you. Importantly progesterone will not prevent all preterm births.
Is there any other way to get progesterone?
Progesterone can also be given vaginally. This would be taken as a pessary placed into the vagina by yourself every night from 16 to 37 weeks of pregnancy.
Your doctor will discuss the best way of taking the medicine with you.
Are there any risks of taking progesterone in pregnancy?
Progesterone medications are thought to be safe for the baby when taken after 12 weeks of pregnancy.
Are there any side effects of taking progesterone during pregnancy?
The injection will be sore.
Your symptoms of pregnancy might become more pronounced with progesterone, such as breast tenderness and nausea.
The use of progesterone injections in pregnancy is quite rare in the UK and so uncommon complications are not as well understood as for common medications. Potential rare complications are: hair loss, breast changes, cervical abnormalities, depression, drowsiness, fever, increased body hair, difficulty sleeping, jaundice (liver problems), nausea, swelling, skin reactions, weight increase.
If you are concerned about a side effect you should seek medical advice from a health professional.
Is progesterone licenced for pregnancy?
Most medications used in pregnancy do not have a licence. There are currently no injections of progesterone with licences for preventing preterm birth in the UK.
To get a licence, the drug company must prove that the medicine works and that it is safe to use, by testing it during clinical trials. The research showing a benefit of progesterone injections in pregnancy is mostly from America. Progesterone injections in pregnancy are licenced for use in America.
As a preterm birth prevention team we feel that the progesterone medication that we are recommending will be of benefit to your pregnancy.
Where can I find out more?
On the March of Dimes website: Progesterone treatment to help prevent premature birth (marchofdimes.org)
-
Omega 3 for women attending the preterm birth prevention clinic
The leaflet is detailed below, or you can download 'Omega 3 for women attending the preterm birth prevention clinic' leaflet in PDF.
What is Omega 3?
Omega 3 is a fatty acid that occurs naturally in foods including fish, eggs and nuts
Why is it important for women attending the preterm birth prevention clinic?
Research published in November 2018 found that Omega 3 supplements can help you have a full length pregnancy. The supplements also help babies to growth to a healthy weight in the womb.
You have been identified as someone who has a higher risk of preterm birth, and so a supplement to prevent preterm birth could be especially helpful in your pregnancy.
What does the research say I should do?
If you are pregnant with one baby, take omega-3 supplements each day starting from around 12 weeks of pregnancy onwards.
- Take at least 500mg of DHA per day.
- This is two tablets of ‘Omacor’ supplements prescribed by the hospital
- You do not need to take more than 1000mg of DHA plus EPA per day. Taking more will not give you or your baby any extra benefit.
- Once you have had your baby you can stop taking omega-3s.
- Continue with your normal pregnancy vitamins too, so long as they do not contain omega 3
*DHA stands for docosahexaenoic acid and EPA stands for eicosapentaenoic acid
How much will this help?
Your doctor will be able to discuss this more fully with you. Omega 3 will not prevent all preterm births.
Can I get the recommended amount of omega-3 fats from foods?
It is difficult to get the recommended amount of the omega-3s docosahexaenoic acid (DHA) and eicosapentaenoic acid (EPA) from food alone, unless you regularly eat fatty fish e.g. salmon, sardines or mackerel.
To get the recommended amount of DHA from salmon, you would need to eat at least 2 large servings (150g) of salmon every week or 3 smaller servings (100g) of salmon every week.
Are there any side effects of taking omega-3 supplements during pregnancy?
Some women may experience fishy burps as a result of taking fish oil supplements. Taking your fish oil supplements with food may help prevent fishy burps.
If you encounter any other side effects, you should seek medical advice from a health professional.
Omega 3 supplements probably increase the risk of needing an induction for a prolonged pregnancy (over 42 weeks of pregnancy). This is much less of a problem for yourself and your baby than a very preterm birth.
What if I’m already taking a pregnancy multivitamin?
If you are already taking a multivitamin supplement, you should check the label to find out how much DHA and EPA the supplement contains. If your pregnancy supplement does contain omega 3 it is normally as a separate tablet.
Most multivitamin supplements do not contain enough omega-3s to reach the amounts recommended to prevent premature birth and you will need to take an omega-3 supplement in addition, to get the 500mg of DHA per day.
Importantly Healthy Start vitamins do not contain Omega 3 at the moment.
We recommend continuing with a pregnancy multivitamin that does not contain omega 3, and taking the prescribed omega 3 supplement as well.
Is omega 3 licenced for pregnancy?
Most medicines used in the UK have a licence that says exactly how the medicine should be used. There are currently no omega 3 supplements with licences for use in pregnancy.
To get a licence, the drug company must prove that the medicine works and that it is safe to use, by testing it during clinical trials. Trials are almost always done with non-pregnant adults first. These trails have shown the omega 3 supplements are safe in non-pregnant adults. The drug companies have not tested whether or not omega 3 is safe in pregnancy.
The research showing a benefit of omega 3 in pregnancy is new (November 2018). The omega 3 medications currently available in the UK are not exactly the same formulations as those used in the research studies. However, they do have the same active ingredients.
Over 5200 pregnant women took part in the research studies showing a benefit in reducing the risk of preterm birth. A large analysis of these studies showed the only negative effect to be an increase in prolonged pregnancy (more than 42 weeks of pregnancy).
Therefore, as a preterm birth prevention team we feel that the omega 3 supplements that we are recommending will be of benefit to your pregnancy.
Where can I find out more?
On the Cochrane website: https://www.cochrane.org/news/new-research-finds-omega-3-fatty-acids-reduce-risk-premature-birth
On the SAHMRI website: https://www.sahmriresearch.org/our-research/themes/healthy-mothers-babies-children/research-list/omega3
- Take at least 500mg of DHA per day.
-
Obstetric Anal Sphincter Injury (OASI)
The leaflet is detailed below, or you can download 'Obstetric Anal Sphincter Injury (OASI)' leaflet in PDF.
What is Obstetric Anal Sphincter Injury?
Obstetric Anal Sphincter Injury (OASI) can extend down from the vaginal wall and backwards through the perineum to the muscle that controls the back passage (anal sphincter).
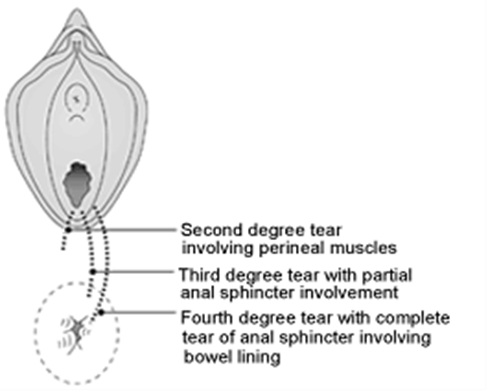
Image Source: The Newcastle Upon Tyne Hospitals NHS Foundation Trust
Why does Obstetric Anal Sphincter Injury occur?
Obstetric Anal Sphincter Injury (OASI) occurs due to the tearing of the tissues during childbirth. It is impossible to predict who will have OASI. However, certain factors increase the chances of a perineal tear happening. These can include:
- First baby
- Ethnicity (Asian and Black)
- Shoulder Dystocia (when one of your baby’s shoulders becomes stuck behind the pubic bone during delivery)
- Large baby
- The direction the baby is facing at birth
- Induction of Labour
- Epidural
- Pushing for a long time
- Assisted delivery
The reported rate of OASI has tripled from 1.8% to 5.9% from 2000 to 2012 in England. The overall incidence in the UK is 2.9%, with a rate of 6.1% in first time mothers compared with 1.7% in those who have had babies before.
How is Obstetric Anal Sphincter Injury repaired?
You will have been examined by a doctor to confirm the extent of your injury. The repair normally takes place in theatre with an anaesthetic. The muscles are stitched back together using dissolvable sutures (stitches).
Care after Obstetric Anal Sphincter Injury?
- To speed up healing and prevent infection keep the area clean.
- Have a tepid bath or shower at least once a day and pat the area dry to keep it free of moisture.
- Change your sanitary pad regularly washing your hands before and after you do so.
- Skin sensation is likely to be altered so do not have too hot a bath.
- Do not put additives such as bubble bath in the water as this may delay healing. You may have heard that salt added to bathwater can help, but salt can make the stitches break down too quickly.
- To avoid pressure on the wound in the first few days it is best to avoid sitting for long periods and to lie on your side. If you are breastfeeding your midwife will show you comfortable positions for you and your baby.
- Signs of infection are an increase in pain, or an offensive discharge. If you experience any of these problems please contact your midwife or GP.
- Constipation causes straining and pressure on the recovering tissues. To help prevent this, please eat plenty of foods containing fibre such as brown rice, cereals and fruit.
- Try to drink about two litres of water each day (if you are breastfeeding increase this to three litres). This helps stools to be softer and therefore easier to pass.
What happens after the repair?
You will be sore but the midwife will be able to give you pain relief, when required. You will be prescribed a set of medication which comprises of:
- A course of antibiotics to prevent infection in your stitches.
- Medicine to prevent constipation (Laxatives) so you are not straining when having your bowels opened.
It may be uncomfortable when you first open your bowels but it will get easier. Don’t be frightened to push down gently so that you can open your bowels - the stitches won’t give way.
Some women have noticed that they have difficulty controlling their bowels at first and some have even leaked, or had problems controlling wind (flatus). If this happens to you, don’t be too worried. This should settle after 2 or 3 weeks when the swelling has gone and the muscles of the back passage start to function properly
Sit on the toilet in the correct position to make sure you empty your bowel properly.
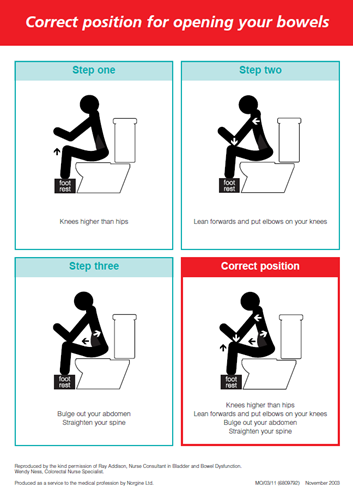
Image Source: Reproduced by the kind permission of Ray Addison, Nurse Consultant in Bladder and Bowel Dysfunction. Wendy Ness, Colorectal Nurse Specialist
Produced as a service to the medical profession by Norgine Ltd.
Is there anything I can do to strengthen the damaged muscles?
YES - Any woman who has had a baby should exercise the pelvic floor muscles. These strengthen the pelvic floor muscles, which have been affected by the tear.
The pelvic floor muscles are the firm supportive muscles that stretch from your pubic bone at the front of your pelvis to the base of your spine at the back. They help to hold your bladder, womb and bowel in place, and to close your bladder outlet and back passage.
When your pelvic floor muscles are well toned they stop leakage of urine from your bladder and wind or stools from the bowel. When you pass urine or stools the pelvic floor muscles relax and afterwards they tighten to restore control. They actively squeeze when you laugh or cough to avoid leaking.
During the first five days the area will feel numb and sore and it will be difficult to exercise during this period, but keep practicing.
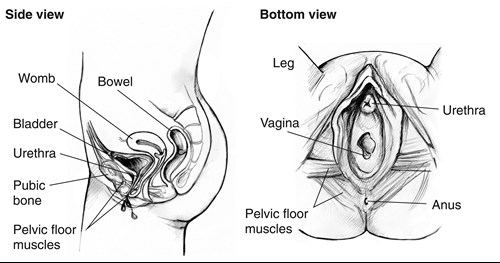
Image Source: National Institute of Diabetes and Digestive and Kidney Diseases
How do I do pelvic floor exercises?
It is not always easy to find your pelvic floor muscles. However, it is important to focus on the right group of muscles when exercising your pelvic floor. You shouldn’t be working the
muscles in your legs, buttocks or above your tummy button and you mustn’t hold your breath. Exercising them should not show at all ‘on the outside’. However, feeling some slight tension in your lower abdominal muscles is normal.
To start exercising lie down with your knees bent and feet on the bed. As you improve you can sit comfortably upright with your feet touching the floor.
Slowly tighten and pull up the muscle around your anus and vagina. This squeezes the muscle upwards and inwards. Imagine that you are trying to stop yourself from passing wind, and at the same time stopping your flow of urine mid-stream. Once you’ve identified the right muscles, try and see what they can do. See how long you can squeeze the muscles for? How many times can you repeat this? Then try and work towards the following routine:
- Squeeze and lift your pelvic floor muscles as hard as you can. Hold for a count of 10 seconds. If your muscles feel too weak to hold for 10 seconds. Aim to build up the time slowly. Repeat this exercise up to 10 times.
- Tighten and lift your pelvic floor muscles as quickly and as strongly as you can, then relax. Do this up to 10 times
- Aim to do the exercises three times a day, every day.
- Squeeze and lift your pelvic floor every time you pick up anything heavyg. baby/ car seat, before coughing/sneezing. This helps your pelvic floor muscles to support the increasing downward pressure on your body.
- Remember to make time for your exercise. Find a time that works for you e.g. when feeding your baby / cuddling baby, resting in bed.
- Persevere with it. Don’t expect it to work instantly. It takes weeks of regular exercise to improve pelvic floor muscles and several months to regain its strength. However, if you stick to the program you should notice a difference after 6 weeks.
If you find the exercises described difficult or not working after six week please speak to your midwife or GP so that they can refer you to a women’s health physiotherapist for further help.
When can I have sex?
When you feel ready and comfortable enough, however, we advise you not to have sex until approximately six weeks, once the vagina has healed and the area feels comfortable. Sexual intercourse may be a little uncomfortable at first, therefore we would advise you to use lubricants which you can buy from most pharmacies. This discomfort should improve with time. If you feel apprehensive about sex or experience pain it is important to speak to the urogynaecology link midwife when you attend the hospital.
DO remember to use effective contraception - as it is possible to conceive a few weeks after your baby is born - See your GP or Family Planning Clinic for contraceptive advice.
What are the long term effects of OASI?
- You may find that you need to rush urgently to the toilet. Some women will experience symptoms such as leakage of urine from the bladder or wind or stools from the back passage. This is often temporary and can improve over time with doing regular pelvic floor muscle exercises. For some women symptoms may appear several months after the repair, in this case seek advice from your urogynaecology link midwife.
- Stitches have usually dissolved by ten days after the birth of your baby. Sometimes a knot of stitch material can persist and cause discomfort. All stitch material used in the repair should eventually dissolve. Often the stitches around the back passage remain in place for up to twelve weeks and can make passing bowel motions uncomfortable. Ensure you do not become constipated and if the pain is intense or you lose blood with the stool seek advice from your doctor.
- Very rarely a connection can form between the vagina and the rectum (rectovaginal fistula). It is important to report any unexpected leakage of faecal material from the vagina to your GP or urogynaecology link midwife. This is not common and can usually be repaired if it does not heal by itself.
Follow up and the Perineal Clinic
An appointment will be sent to you to attend the Perineal Clinic for approximately 6-8 weeks after your delivery. This clinic is held in the Urogynaecology Department, which is located on the ground floor of the hospital.
The Perineal clinic is a specialist clinic for women who have had OASI or who have developed chronic perineal problems post-delivery.
The first appointment will be with the Urogynaecology Link Midwife. The midwife will ask you some questions regarding any bladder or bowel symptoms you may have experienced and examine the perineum and pelvic floor muscles. This is to assess that your bowels, bladder and pelvic floor muscles are functioning normally and that your perineum has healed. You can decline this examination if you wish.
Prior to the appointment you will be sent a special on-line questionnaire (ePAQ) to complete as part of you medical care. This is confidential. Please try and complete it before attending for the appointment.
As part of your follow-up we will arrange for you to re-attend the clinic at approximately 6-9 months after your delivery for some Anorectal studies. These are useful to check how well the muscle in the back passage has healed and how well it is working. You will be asked to complete another ePAQ prior to this appointment. You will be seen by one of the Consultants following the tests to discuss the results.
It is very important that you attend for both these appointments.
What if I do not want to have the tests?
The tests do give us useful information about how well you have recovered from the tear and can help us in providing you with a clearer picture of the future with regards to your continence. They are also very useful, as the consultant can help advise you on how she would recommend you deliver any future pregnancies based on the test result. However, if you do not want to have the tests done, please tell the midwife.
What about future deliveries?
It is not known what happens to the anal sphincter muscles in the long-term, after this type of damage. After the Anorectal studies, we will have a better idea of how successful the repair has been. If there are no symptoms and no damage evident, it may be possible for you to consider future vaginal delivery. This causes a 25 in 100 risk of worsening the previous damage. If there are symptoms or evidence of persistent damage then your obstetrician may recommend elective (planned) caesarean section in a future pregnancy.
If you have any questions, please contact the Urogynaecology Specialist Midwife on 0151 708 9988 Ext. 4321
Some useful websites are:-
-
Postnatal Urinary Retention
The leaflet is detailed below, or you can download 'Postnatal Urinary Retention' leaflet in PDF.
What is postnatal urine retention?
We want you to be able to pass urine spontaneously within 4 hours of your baby being born or 4 hours after you have had your catheter removed. If you are unable to do this it may mean you have gone into postnatal urinary retention. Sometimes you may not be able to pass urine at all but sometimes you may be able to pass small volumes of urine with difficulty, but larger volumes still remain in your bladder. If this happens it is important to tell your midwife.
Why does urine retention happen?
- This can happen because you feel sore underneath, especially if you have had stitches
- There is usually some swelling in and around the vagina after having your baby, which can take time to settle and can make it harder for you to pass urine
- An epidural or spinal anaesthetic can cause altered sensation in your lower body, which can affect your bladder temporarily
- There may be injury to the pelvic nerves, which may have happened during the birth
You are more likely to have problems if:
- This is your first baby
- You have had an epidural or spinal anaesthesia
- You have had a prolonged labour
- You have had an instrumental delivery (forceps or ventouse)
- You have had a tear or stitches
- You have a urine infection
- You have had problems previously
What can I do to help me try to pass urine?
- Analgesia – ask your midwife to give you painkillers if you feel sore
- Getting up and walking about – movement really helps to reduce any swelling there may be
- Privacy – If you feel nervous about using the toilet in the bay, use one of the toilets on the main corridor of the ward
- Taking a warm bath or shower – this will help relax you and make you more comfortable
What happens if I can’t pass urine?
If you are unable to pass urine 4 hours after having your baby or your catheter removed then a midwife or doctor will scan your bladder to check how much urine is there. It may be likely that the midwife will then need to empty your bladder using a catheter.
If you are in discomfort from a full bladder before this time or the midwife can feel a very full bladder, then you may have to have your bladder emptied earlier.
What is a catheter?
This is a thin, sterile tube, which is usually made of plastic. The catheter is passed into your urethra (the small opening through which urine is passed) and into your bladder. This allows the urine to drain out. Your midwife or doctor will ask for your consent to put a catheter in your bladder. If you decide you do not want this, then you will be encouraged to try to pass urine again yourself. You could be at risk of harming your bladder in the long term if you still cannot pass urine, especially if there is a large volume of urine there.
Having a catheter inserted can be a little uncomfortable but it is a quick, safe procedure .You should feel much more comfortable when your bladder is emptied. It may be necessary to leave the catheter in place for at least 24 hours, to let the bladder “rest”. If this happens, a leg drainage bag will be attached to the catheter to collect the urine. This will be strapped to your leg to allow you to continue to mobilise. Staff will show you how to empty your bag when it is getting full. Overnight, another larger catheter bag will be attached to the leg bag and kept on a stand at the side of the bed. This will allow more urine to drain without having to be emptied as frequently and therefore allow you to rest for longer periods.
You can still have showers and it is important to keep the perineal area (the area between the vagina and back passage) clean, especially after opening your bowels.
It is really important to stay hydrated. Aim to drink 2 litres of water or dilute juice per day, 3 litres if breast-feeding.
What happens when the catheter is removed?
You will be asked for permission to take your catheter out. A midwife or maternity assistant will remove it. This is a quick procedure and you may experience some very slight discomfort.
It is important that when the catheter is removed we monitor what you drink and how much urine you pass. This can tell us whether your bladder is working normally again. This is easy to do: you will be given a fluid chart and shown how to write down what you drink and how much urine you pass. To measure the urine you pass, your midwife or maternity assistant will provide you with a jug.
You may find that initially you are unable to tell when your bladder is full. This is usually a temporary problem. If this is happening then it is recommended that you try to go to the toilet every 3-4 hours. This will prevent your bladder getting too full.
What happens if I cannot pass urine after the catheter is removed?
It may be necessary to put the catheter back in. This would be for around a week and you would then be referred to the link Midwives in the Urogynaecology Department. This is situated on the ground floor of the hospital. The staff there are trained to provide specialist investigation, advice and support for women with bladder problems. They will discuss the best form of management for your bladder problem.
In most cases, urine retention is a temporary problem, which may take a few weeks to resolve. If you have any ongoing voiding issues we may teach you how to perform self catheterisation (Clean Intermittent Self Catheterisation) as an interim measure until the issues resolves. The staff in the Urogynaecology department will provide support and advice during this time and will arrange any follow-up you may need.
Will bladder problems happen again in another pregnancy?
This is hard to say – there is a chance you may have a recurrence of these problems however we cannot predict if this would be the case for you. If you fall pregnant again, make sure you tell the midwife who is ‘booking’ you in that you have had previous bladder problems with your last pregnancy, so that the staff caring for you are aware.
Many women have temporary bladder problems in pregnancy and after childbirth, please do not feel embarrassed to discuss any problems with your midwife or doctor who can offer advice and support.
If you have any questions, please contact the Urogynaecology Link Midwives on 0151 702 4321
For more information:-
www.bladderandbowelfoundation.org
Please note that Liverpool Women’s NHS Foundation Trust is a smoke free site. Smoking is not allowed inside the hospital building or within the hospital grounds, car parks and gardens.
Staff are available to give advice about stopping smoking, please ask your Nurse or Midwife about this.
-
Twin to Twin Transfusion Syndrome
The leaflet is detailed below, or you can download the 'Twin to Twin Transfusion Syndrome' leaflet in PDF.
Twin to Twin Transfusion Syndrome
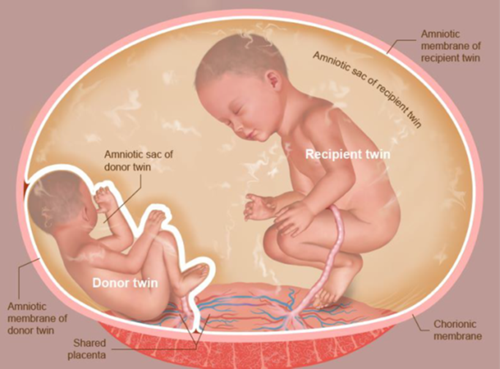
A diagnosis of Twin to Twin Transfusion Syndrome (TTTS) can be an upsetting and emotional time for you and your family. TTTS is a complication that occurs in around 10-15% of pregnancies to twins that share a placenta (monochorionic). It can occur at any time during your pregnancy but is most likely to occur in the early to middle stages of your pregnancy before 26 weeks.
This leaflet has been produced to give you a bit more information about TTTS and can be used alongside the advice and support you will receive from the Liverpool Multiple Pregnancy Team
What is TTTS?
TTTS occurs when there are abnormal connections between the babies’ blood vessels on the surface of the placenta. This then causes blood to be transferred (shunted) from one twin (called the donor) to the other (the recipient).
By donating some of its blood supply to its sibling, the donor has less oxygen in its blood. As the donor has less oxygen it prioritises the flow of blood to the brain. This may mean that other organs such as the kidneys do not receive as much blood which will reduce urine production and lead to a small bladder and less fluid around the baby. We can see this on ultrasound.
The recipient twin has an increase in blood volume from the donor which can sometimes put strain on the baby’s heart as it must pump harder. The recipient will compensate for the extra blood by producing more urine, increasing the amount of fluid around the baby.
How is TTTs diagnosed?
TTTS is diagnosed by ultrasound scan and divided into stages. Early ultrasound scanning is important to determine the type of twin pregnancy and whether the babies share a placenta.
You will have regular ultrasound scans in pregnancy to screen for TTTS. The diagnosis is made by measuring the amount of fluid around each baby, the size of their bladders, the baby’s weight and the baby’s blood flows (Dopplers).
There are a few warning symptoms to keep an eye out during your pregnancy but often you will have no symptoms at all:
- Sudden weight gain
- Feeling of increased pressure in your tummy
- Feeling like your tummy is tight
Quintero Stage
Key Features
Treatment indicated
1
Low liquor around the donor and high around the recipient
No
2
No urine in the donor baby’s bladder
Yes
3
Abnormal blood flow (Doppler) in either baby
Yes
4
Heart failure or hydrops (fluid inside the baby’s tummy) in the recipient baby
Yes
How is TTTs managed?
If you are diagnosed with TTTS, you and your babies will be monitored very closely. Every pregnancy is different, and a specialised plan will be made with you and the Liverpool Multiple Pregnancy Team.
If the TTTS is mild (stage 1) and the babies are stable, you may not need any treatment. You will be regularly monitored and if the situation gets worse, doctors may intervene.
If the TTTS is more advanced you will be advised about treatment options. If no treatment is performed the outcome for the pregnancy can be poor with an 80% chance of losing at least one baby. The most effective treatment is Laser Ablation of the blood vessels of the placenta which connect the babies. It involves a needle being inserted into your uterus (womb). The laser will burn the connecting blood vessels stopping the shunting which causes the TTTS. Both babies will still be connected to the placenta by their umbilical cords so will still receive nutrients and blood.
Laser for TTTS is our most effective treatment with a 75% chance of taking home one or both babies, 50% chance of taking home both. However, there are complications associated with laser, such as; preterm labour, rupture of membranes and have learning difficulties after birth.
How and when will my babies be delivered?
TTTS is associated with premature labour and therefore your babies may need to spend some time on the neonatal unit. If the TTTS is fully resolved the pregnancy may carry on as normal with delivery planned as for any other monochorionic twin pregnancy and a vaginal delivery may be possible.
Key websites to visit
Twins Trust (formerly TAMBA)
twinstrust.org
YouTube Video
-
Stopping Smoking in Pregnancy
The leaflet is detailed below, or you can download the Stopping Smoking in Pregnancy leaflet in PDF.
This information is for you if you smoke and are either already pregnant or thinking about having a baby. It is also for you if you are exposed to tobacco smoke at home. You may also find it helpful if you are the partner or a relative of a woman who smokes.
Many women find it difficult to stop smoking but it is one of the most important things you can do to improve your baby’s health, growth and development. It is also the single most important thing that you can do to improve your own long-term health.
This leaflet tells you about the effect of smoking on you and your baby. It also tells you about the help and support that you will be offered to stop smoking. It’s never too late to stop smoking and your healthcare team will be supportive throughout your pregnancy.
When you stop smoking, you and your baby will feel the benefits immediately.
Why is smoking in pregnancy harmful to me and my baby?
Just as smoking is bad for you, babies in the womb can be harmed by tobacco smoke because it reduces the amount of oxygen and nutrients that pass through the placenta from you to your baby.
Smoking when you are pregnant increases your risk of:
- Miscarriage
- ectopic pregnancy (a pregnancy growing outside the womb)
- Your baby dying in the womb (stillbirth) or shortly after birth – one-third of all deaths in the womb or shortly after birth are thought to be caused by smoking
- Your baby being born with abnormalities – face defects, such as cleft lip and palate, are more common because smoking affects the way your baby develops
- Your baby’s growth and health being affected – the more you smoke, the less healthy your baby will be, and a baby that is small due to smoking is more likely to have health problems when young and also later in life
- Bleeding during the last months of pregnancy, which is known as an abruption (when the placenta comes away from the wall of the womb) – this could be life threatening for you and your baby
- Premature birth, when you have your baby before 37 weeks of pregnancy.
Babies and children whose mothers smoke during pregnancy are also at greater risk of:
- Sudden and unexplained death, known as sudden infant death syndrome (SIDS) – as well as happening to new born babies, this can also happen to infants over 12 months: the risk is greater if you or your partner continue to smoke after she or he is born, particularly if you share a bed with your baby at night
- Asthma, chest and ear infections, and pneumonia
- Behaviour problems such as ADHD (attention deficit hyperactivity disorder) performing poorly at school.
STOPPING SMOKING REDUCES ALL OF THE RISKS DESCRIBED ABOVE.
Will I be asked about smoking when I am pregnant?
Yes. From your first antenatal appointment, your midwife will ask whether you or any other member of the household smokes. This is important so that you and your family can be given support and help to stop smoking as early as possible. You will be asked how often you smoke and how much tobacco you smoke per day. You will be given information about how smoking and passive smoking harms you and your baby (see next section).
In an effort to support you and reduce smoking in pregnancy, to give you and your baby the added benefits of a smoke free pregnancy – all women who smoke, e-cig and vape are referred to our local stop smoking service. The Stop Smoking Advisor will contact you and offer further support and advice.
Second-hand (passive) smoke harms your baby.
If your partner or anyone else who lives with you smokes, their smoke can affect you and your baby before and after their birth. You may also find it more difficult to stop if someone around you smokes.
Second-hand smoke can also reduce your baby's birthweight and increase the risk of sudden infant death syndrome (SIDS), also known as "cot death". Babies whose parents smoke are more likely to be admitted to hospital for bronchitis and pneumonia during their first year.
To find out more about quitting and to get support, your partner can call NHS Smoke free helpline on 0300 123 1044 from 9am to 8pm Monday to Friday, and 11am to 4pm Saturday and Sunday
I’m a smoker, so what should I do?
There is no safe level of smoking, either for you or your baby. The earlier you stop smoking, the greater the benefit to you and your baby, but it is important to know that stopping at any time during pregnancy is beneficial to some extent.
Reducing the number of cigarettes you smoke is a positive step, although there is no evidence that this is better for your baby. Therefore, both you and your partner will be advised to stop completely – not just cut down. To help you with this, you should be referred to services that will help you both to stop smoking (see information at the end of the leaflet).
What is the carbon monoxide (CO) test?
Carbon monoxide (CO) levels are higher in women who smoke and in passive smokers than in women who don’t. CO is a poisonous gas that restricts the amount of oxygen getting to your baby.
At your first antenatal appointment your midwife will ask you to do a breath test, which will measure your level of exposure to CO. This will help your midwife measure your exposure to tobacco smoke. This will also be repeated when you are 36 weeks pregnant and some other times it may be required in pregnancy.
All pregnant women are advised to have the test whether they smoke or not as levels may also be high if you have faulty gas appliances at home. CO poisoning can be fatal. If you don’t smoke and you are not exposed to tobacco smoke but your levels are high, you should contact the free Health and Safety Executive Gas Safety Advice Line on 0800 300 363. CO levels may also be raised if you are exposed to high levels of pollution or if you have a medical condition called lactose intolerance.
Nicotine replacement therapy
You can use nicotine replacement therapy (NRT) during pregnancy if it will help you stop smoking and you're unable to stop without it. It's not recommended that you take stop smoking tablets such as Champix or Zyban during pregnancy.
NRT contains only nicotine and none of the damaging chemicals found in cigarettes, so it is a much better option than continuing to smoke. It helps you by giving you the nicotine you would have had from a cigarette.
You can be prescribed NRT during pregnancy by a GP or an NHS stop smoking adviser. You can also buy it over the counter without a prescription from a pharmacy.
NRT is available as patches, gum, inhalator nasal spray, mouth spray, oral strips, lozenges and microtabs.
If you have pregnancy-related nausea and vomiting, patches may be a better solution.
NRT patches should be used for no more than 16 hours in any 24-hour period. The best way to remember this is to remove the patch at bedtime.
Before using any of these products, speak to a midwife, GP, a pharmacist or a specialist stop smoking adviser.
By getting this specialist advice you can be sure that you're doing the best for your baby and for you.
Call the NHS Smokefree helpline on 0300 123 1044 from 9am to 8pm Monday to Friday, and 11am to 4pm Saturday and Sunday.
Remember, you are twice as likely to be successful at quitting if you get some support from a trained adviser.
E-cigarettes and Vaping in Pregnancy.
E-cigarettes are fairly new and there are still some things we do not know. However, current evidence on e-cigarettes indicates they are much less risky than smoking.
Cigarettes deliver nicotine along with thousands of harmful chemicals. E-cigarettes allow you to inhale nicotine through a vapour rather than smoke. By itself, nicotine is relatively harmless.
E-cigarettes do not produce tar or carbon monoxide, the 2 main toxins in cigarette smoke. Carbon monoxide is particularly harmful to developing babies. The vapour from an e-cigarette does contain some of the potentially harmful chemicals found in cigarette smoke, but at much lower levels.
If using an e-cigarette helps you to stop smoking, it is much safer for you and your baby than continuing to smoke.
Unlike nicotine replacement therapy (NRT), such as patches or gum, e-cigarettes are not available on an NHS prescription. If you want to use an e-cigarette, you can still get free expert help from a stop smoking adviser.
Call NHS Smokefree helpline on 0300 123 1044 for more information, or ask a midwife to refer you.
Find out more about using e-cigarettes to stop smoking.
NHS Smokefree Helpline.
The NHS Smokefree helpline offers free help, support and advice on stopping smoking and can give you details of local support services.
You can also sign up to receive ongoing advice and support at a time that suits you.
Information:
NHS Smokefree helpline: 0300 123 1044
9am to 8pm Monday to Friday
11am to 4pm Saturday and Sunday.
To find your nearest NHS Stop Smoking service talk to:
- a midwife
- a health visitor
- a nurse at your GP surgery
- a pharmacist
NHS Stop Smoking services can offer 1-to-1 or group sessions with trained stop smoking advisers and may have a pregnancy stop smoking specialist.
They can also offer advice about dealing with stress, weight gain and support the use of NRT (such as patches or gum), if appropriate, to help you manage your cravings.
Further Support and Advice.
Smokefree Liverpool
Life Bank 23 Quorn Street
Kensington
0800 061 4212
0151 374 2535
Text QUIT to 66777
Please speak to your Midwife or G.P about the benefits to stopping smoking in pregnancy and for further information on accessing stop smoking services.
The information found in this leaflet is taken from www.nhs.uk
and
www.rcog.co.uk Smoking and Pregnancy Leaflet, produced Dec 2015. Accessed 16.01.2019
This leaflet can be made available in different formats on request. If you would like to make any suggestions or comments about the content of this leaflet, then please contact the Patient Experience Team on 0151 702 4353 or by email at pals@lwh.nhs.uk
Liverpool Women’s NHS Foundation Trust
Crown Street
Liverpool
L8 7SS
Tel: 0151 708 9988
Issue Date: 18.06.2020
Review Date: 18.06.2023
Ref: mat/2020-282-v1
© Liverpool Women’s NHS Foundation Trust
-
Ondansetron in pregnancy
The leaflet is detailed below, or you can download 'Ondansetron in pregnancy' leaflet in PDF.
What is Ondansetron?
Ondansetron is a medication that we use to treat nausea and vomiting. In pregnancy it is used as third line medication. This means that it is used if two other medications have not helped with the woman’s symptoms.
Is Ondansetron safe in pregnancy?
A large study of over 1.8million pregnancies in 2018 has shown that there is no increased association with heart problems in babies of mum’s who take Ondansetron in pregnancy. There was an increased association of 3 per 10,000 of cleft palate. This means that the number of babies born with cleft palate increased from 11 per 10,000 to 14 per 10,000).
What are the benefits of taking Ondansetron in Pregnancy?
There is a significant risk to women in early pregnancy with severe nausea and vomiting, including and not limited to malnutrition, dehydration, hospital admission, loss of work, blood clots, reduced quality of life, small babies and some women opt to terminate the pregnancy as the sickness is so severe.
Because we use Ondansetron as a third line this means that only women with severe nausea and vomiting are taking the medication.
What does the Pregnancy Sickness Community say?
The pregnancy sickness community has challenged this view that Ondansetron should not be used in the first trimester based upon the trial. The European Medicines Agency (EMA) responded to say that their statement is not referring to women with severe nausea and vomiting in pregnancy. They said that it is up to local units to decide whether to continue to prescribe for women with severe nausea and vomiting in pregnancy.
The advice from the pregnancy sickness community is that we should inform women of the small increased association with cleft lips and palates . If women understand and are willing to accept the risk we should continue to prescribe Ondansetron.
More information
Talk to your doctor for more information or visit the Pregnancy Sickness Support website https://www.pregnancysicknesssupport.org.uk/
i Huybrechts K F, Hernandez-Diaz S, Straub L, Gray K J, Zhu Y, Patrono E, Desai R J, Mogun H, Bateman B T. Association of maternal first trimester Ondansetron use with cardiac malformations and oral cleft palates in offspring. JAMA 2018:320(23);2429-2437
ii Ondansetron update. Pregnancy Sickens Support. Available at https://www.pregnancysicknesssupport.org.uk/news/items/ondansetron-update Accessed 28th November 2019This leaflet can be made available in different formats on request. If you would like to make any suggestions or comments about the content of this leaflet, then please contact the Patient Experience Team on 0151 702 4353 or by email at pals@lwh.nhs.uk
-
Latent Phase of Labour - How will I know my labour has started?
The leaflet is detailed below, or you can download the 'latent phase of labour' leaflet in PDF
Labour is a journey and every woman’s journey is different. This leaflet has been produced by midwives to try to help you help yourself during the early stages of labour.
We hope that using some of the tips in this leaflet will help.
Coping with the Latent Phase of Labour
The three stages of labour
The first stage
Is the longest stage and ends when the neck of your womb opens fully (10 centimetres dilated)
The second stage
Is when your baby moves down through the birth canal and is born.
The third stage
Is when your afterbirth is delivered.
What is the Latent Phase of Labour?
The latent phase of labour is the very first part of your labour. During pregnancy the neck of the womb (cervix) is long, firm and closed.
During the latent phase the neck of the womb shortens (effaces) and opens (dilates) to about 4 centimetres.
The next part of labour is called active labour and we say labour has become established or properly started.
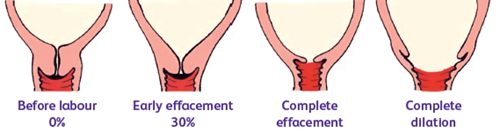
What happens during the latent phase?
During the latent phase the muscles of the womb (uterus) contract and this causes the neck of the womb to shorten and open by 4 centimetres. The latent phase can last several days. Some women feel backache or cramps during this time. Some women will have bouts of contractions lasting a few hours. The contractions may start and stop several times. This is normal.
Many women pass a “show”, which is a plug of mucous from the neck of the womb, usually stained with blood. Some women pass a large plug of mucous all at once; others have several “shows” over several days.
In the latent phase of labour contractions can vary in length and how often they come. They may continue for several hours but not become much longer and stronger. This is also normal.
If your contractions do slow down or stop, this is a good time to rest and make sure you have something to eat. When your body has built up some energy supplies your contractions will start again. Many women find that coming into the hospital or having a vaginal examination during the latent phase slows down the contractions; this is why your midwife may encourage you to remain at home in early labour or avoid too many internal examinations.
THIS START-STOP PATTERN IS COMMON
In the active phase of labour contractions change, they become
LONGER, STRONGER AND CLOSER TOGETHER
and usually continue to become stronger until the baby is born
It is very important you have a supportive birthing partner with you. This should be someone who is happy to be with you throughout your labour. Choose someone who has a positive attitude about birth and who you feel totally relaxed, confident and comfortable with.
We welcome two birthing partners (occasionally there may be times when this is not possible- please check hospital website or speak to your midwife for more information)
What can I do in the Latent Phase of Labour?
It is best to try and stay as relaxed as you can, distract yourself from focusing on the contractions. It is a good idea to stay at home for as long as possible. This is because there is evidence that if you arrive in hospital in established (strong) labour you are more likely to have a straight forward birth.
You may also feel more relaxed and comfortable in your own home.
There are many things you can do to help your labour go well
Things to try:
- Potter around the house
- Take a walk
- Watching a DVD/video (one that makes you laugh is best)
- Take a warm bath or shower
- If the contractions slow down or stop, have a short nap or lie down
- Do some relaxation
- Keep your breathing quiet and sigh out slowly during contractions
- Ask your birth partner to give you a massage
- Kiss and cuddle or make love
- Use your TENS machine if you plan to use one
- Put a heat source, wrapped in a small towel on areas that ache
- Keep upright and mobile
- Change your position frequently
- Try a birthing ball
- Drink plenty of fluids
- Eat little and often – carbohydrates like bread or pasta and sugary foods
Remember
You should inform a midwife if you experience
- Constant or rapidly increasing pain
- You know or suspect your waters have broken
- You have a green or yellow vaginal discharge
- Vaginal bleeding that is not mucousy (jelly-like)
- Any change in your baby’s movement pattern – Your baby’s movements should continue throughout labour
- Persistent vomiting
- Feeling generally unwell or feverish
- You need further advice or reassurance
If you think you may be in early labour, call the Triage Midwife at the hospital for advice.
If you have any pregnancy complications please inform the midwife you speak to.
If you are not in established (strong) labour when you are assessed by a midwife you may be advised to stay at home.
Research tells us that women who spend the early part of their labour at home are less likely to experience medical interventions such as caesarean section, a drip to speed up labour, or develop an infection.
If you have signs of labour or are concerned please speak with a midwife:
Call our Triage Midwife on 0151 702 4413
Or
The Midwife Led Unit on 0151 708 9900
-
Obstetric Cholestasis
The leaflet is detailed below, or you can download the 'Obstetric Cholestasis' leaflet in PDF.
What is Obstetric Cholestasis?
Obstetric cholestasis also known as ICP (Intrahepatic Cholestasis of Pregnancy) is the commonest liver condition specific to pregnancy
It affects more than 5,000 women a year in the UK
Its cause is unknown, but is thought to be a combination of:-
- Genetics – it can run in families
- Hormones – it is more common in twins/multiple pregnancies
- Environment
Cholestasis causes itching. Itching more commonly affects the hands and feet, but can occur anywhere on the body. It can vary from mild to severe. Most women notice itching is worse at night.
Why is ICP important?
ICP is associated with increased risk of
- Baby passing meconium (poo) prior to birth
- Spontaneous preterm (early) labour
- Admission to neonatal units
- Stillbirth (small risk applies to women with severe ICP with bile acids more than 100)
Most recent research has suggested that 90% women can be reassured that risk of stillbirth for their baby is not increased due to the condition.
Careful monitoring and management of the 10%, who are at risk, can mean babies can be born safely.
Diagnosis and management of obstetric cholestasis
20% of women will experience itching during pregnancy, but only a small number will have ICP.
The most important test is a blood test for Bile Acids. This is done alongside liver function tests (LFTs).
If this test is normal and itching persists it should be re-checked, as the itch can be present for weeks before it becomes raised.
Treatment of cholestasis involves
- Medicines to help with itching (antihistamines and topical treatments such as creams)
- Regular blood tests. Frequency will depend on how pregnant you are and blood levels.
- Early delivery of baby (between 35 and 39 weeks) dependent on bile acid levels.
After birth
After birth blood tests should go back to normal after 6 weeks. It is important that your GP checks this as if they remain abnormal you might need to be referred to a liver specialist
Having cholestasis means you have a higher chance of developing liver problems such as gallstones in the future
Up to 80% women will have cholestasis in a following pregnancy
Further information and support available from
-
My Pregnancy Notes Information Leaflet
The leaflet is detailed below, or you can download 'My Pregnancy Notes' leaflet in PDF.
The new way to view and interact with your maternity notes online
Registering for My Pregnancy Notes
You will only ever need to register for My Pregnancy Notes once. If you ever get pregnant again and wish to have your care with us, you will be able to create a new pregnancy linked to your account.
- Open web browser on PC/Tablet/Phone
- launch mypregnancynotes.com

- Click Register
- Click I am a pregnant woman
- Complete registration Details
- Your email will become your username
- Click Verify Email
- Navigate to your email
- Open email
- Click Verify Email
- Create Password
- Click Complete Registration
- You will be asked to complete a registration form for this pregnancy
- Click Complete Registration
- Complete form
- Select Liverpool Women’s Hospital
- Complete data sharing consent (if you do not wish to share data please discuss this with your midwife. What your data is used for will be discussed with you).
- Click Submit
What can I do on My Pregnancy Notes?
My Notes:
- Welcome page with advice on when to call your midwife courtesy of MAMA Academy.
- Add information to your notes including questions or maternity certificates.
My Health:
- Record a private diary and
- Add observations if you have been asked to by your clinician.
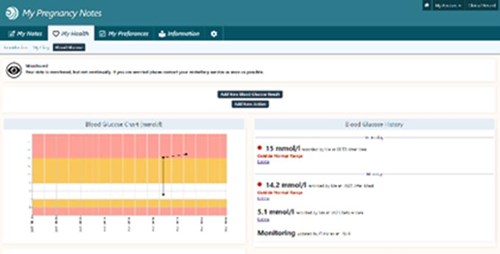
My Preferences/information and Settings:
- Add in preferences for your pregnancy and birth.
- Access information leaflets and links.
- Take control of some of the things you see in your notes.
Why should I use My Pregnancy Notes?
We have been working very with hard other hospitals to produce a tool which you can use to access your notes wherever and whenever you wish and communicate better with your clinicians.
My Pregnancy Notes will allow you to be more involved in your care and provide your clinicians with more information than ever about you preferences. It will enable you access to up to date information about your care and the leaflets and information you need, whenever you need it.
Your clinician may also discuss the need to monitor a part of your care (Blood pressure, Temperature etc.). If this is the case, they will discuss this with you, and you will be able to enter these observations straight into your notes, which can be seen in real time by your clinician.
What if I need help?
If you need help, the first person to contact should always be your midwife or doctor giving your care. However below there are links to help guides to help you with the use of My Pregnancy Notes.
User Guides
https://help.k2ms.com/portal/kb/hampton-blood-pressure-mo

Patient Information
https://help.k2ms.com/portal/kb/hampton-blood-pressure-monitoring/general/patient-informationhy

Add My Pregnancy Notes to your phone home screen
- Open web browser
- Launch mypregnancynotes.com
iOS (Safari)
Select the action button highlighted in green below

- Scroll down and select add to home screen
- Click add
Android (Chrome)
- select the action button highlighted in green below

- Click add
Contact Us
Liverpool Women's NHS Foundation Trust
Crown Street
Liverpool
L8 7SS0151 708 9988

-
Asprin in Pregnancy to prevent Pre-Eclampsia
The leaflet is detailed below, or you can download 'Asprin in Pregnancy to prevent Pre-Eclampsia' leaflet in PDF.
You have been asked to take 150mg of Aspirin during your pregnancy to reduce the risk of Pre-Eclampsia.
This leaflet explains why we have asked you to take Aspirin during your pregnancy.
What is Pre-Eclampsia?
Pre-Eclampsia is a condition found only in pregnancy that causes:
- Raised blood pressure (Hypertension)
- Protein in the urine (Proteinuria)
It affects around 2 to 10 of every 100 pregnant women. Most women will have a mild form, with some having more severe cases.
Women will often have no symptoms, and it is diagnosed at routine antenatal appointments with your midwife. Some women will experience headaches, blurred vision and swelling of the hands, feet and face.
These symptoms can be managed with medications that bring your blood pressure down, however the only cure for pre-eclampsia is when your baby is delivered.
What is the risk of Pre-Eclampsia?
If pre-eclampsia is not treated then there is a risk that it may affect the growth of the baby inside the womb, as well as a risk to the health of the mother. In these cases, you may be advised to have baby delivered earlier.
Who gets Pre-Eclampsia?
Any woman can develop pre-eclampsia during pregnancy. However, some women are at increased risk for a variety of reasons. The risk factors are divided into Moderate Risk Factors and High-Risk Factors.
Moderate Risk Factors:
- First pregnancy
- BMI >35
- Age >40 years
- Multiple pregnancy (twins/triplets etc)
- Family history of pre-eclampsia (Sister/Mother)
- >10 years since previous pregnancy
- If you have a British and Minority Ethnic Origin (BAME)
High Risk Factors:
- Previous hypertensive disease in previous pregnancy
- Pre-existing chronic or essential hypertension
- Chronic kidney disease
- Systemic Lupus Erythematosus or Antiphospholipid antibody syndrome (Autoimmune disease)
- Diabetes
- Previous fetal growth restriction (birthweight less than the 3rd centile) at any gestation
- Low PAPP-A on 1st trimester combined (0.41MoM)
Why have I been asked to take Aspirin?
You have been asked to take Aspirin because your doctor feels that you are at risk of developing pre-eclampsia based on the previously mentioned risk factors. Research suggests that taking Aspirin during pregnancy reduces your risk of developing pre-eclampsia before 37 weeks by two thirds. However, aspirin will not prevent all cases of pre-eclampsia.
Is Aspirin safe to take during pregnancy?
Yes, it is.
Research has shown that Aspirin does not cause harm to the development of the baby during pregnancy. There is also no increased risk of bleeding when taking Aspirin during pregnancy, either to you or the baby.
Although it is advised for you to take Aspirin, it is an unlicensed use of the medication, therefore needs to be prescribed by a doctor.
Are there any side effects?
Like all medications, aspirin can cause side effects, although not everyone gets them.
Common Side effects
- Mild indigestion – taking aspirin with or just after food is less likely to upset your stomach. If you also take indigestion remedies, take them at least two hours before or after you take your aspirin.
Rare Side effects
- Allergic reaction – as with all medications there is a chance you may have an allergy to this. If you experience wheezing, sweeling of the lips, rashes, stomach pains or vomiting blood please seek medical assistance immediately.
Can I take low dose aspirin?
Although low dose aspirin has its benefits in those at risk, it is not suitable for everyone.
Please tell your midwife / obstetrician or GP if you have any of the below.
- Bleeding disorders – In some bleeding disorders aspirin may be contra-indicated, if there is uncertainty this can be discussed with the haematology team
- Severe asthma
- Allergy to aspirin / NASID’s – you may have previously been old to avoid this type of medication.
What happens next?
We recommend you take 150mg (2x75mg tablets) of Aspirin every night from the 12th week of pregnancy. You should start taking this before 16 weeks gestation, starting aspirin after this gestation may not help in the prevention of pre-eclampsia. It is best to take in the evening either with or just after food. Please do not worry if you forget to take a tablet, just take one when you remember, however make sure you only take 150mg once a day. We will ask your GP to provide a prescription for Aspirin and we will continue to monitor your blood pressure and urine protein throughout your pregnancy. You can stop taking the aspirin at 36 weeks. If you think you may be in labour, you can stop taking your aspirin until this is confirmed. It will not increase your risk of bleeding during your labour.
Further information
If you have any further questions about taking Aspirin during pregnancy, or about pre-eclampsia, then please speak to your community midwife, GP or contact the Antenatal Clinic at Liverpool Women’s Hospital.
Best Use of Medicines in Pregnancy website: www.medicinesinpregnancy.org NHS website: www.nhs.uk/medicines/low-dose-aspirin
NHS website: www.nhs.uk/medicines/low-dose-aspirin
NICE Guideline, Hypertension in pregnancy: diagnosis and management
-
High Blood Pressure and Pre-eclampsia
The leaflet is detailed below, or you can download 'High Blood Pressure and Pre-eclampsia' leaflet in PDF.
This leaflet is for women who had high blood pressure (hypertension) in pregnancy or shortly after delivery.
Women who had raised blood pressure during pregnancy, have a greater risk of health problems in future pregnancies and in later life. This risk can be reduced by making healthy lifestyle choices and having regular check-ups with your GP (family doctor). Most women will have their follow up appointments with their midwife and GP.
You should have a follow-up appointment with your healthcare professional 6–8 weeks after giving birth. If you are still on medication to treat your blood pressure at this stage or if there is still protein in your urine, you may be referred to a specialist for further investigations.
If you are concerned about your blood pressure or feel unwell, and your baby is less than four weeks old, please contact your community midwife (using the contact details provided by the hospital).
If your baby is four weeks old or more, please contact your GP.
Why worry about pre-eclampsia and high blood pressure after birth?
Although pre-eclampsia is usually considered a disease of the second half of pregnancy, it can show itself for the first time after delivery. Pre-eclampsia at any time can cause headaches, visual disturbances, nausea and vomiting and other unpleasant symptoms.
High blood pressure can cause cerebral haemorrhage (a stroke) if not treated.
Eclamptic fits can occur up to 23 days postnatally, and long term untreated high blood pressure can lead to heart and blood vessel problems.
Facts about pre-eclampsia after the baby is born
- Pre-eclampsia always goes away eventually after the baby is born because it is a disease of the placenta (afterbirth).
- It may disappear within hours, or any time up to six months after the birth.
- Pre-eclampsia can present for the first time after birth, around 1 in 3 cases develop in the post natal period
- Pre-eclampsia can present up to 4 weeks postnatal
- Pre-eclampsia may necessitate a longer postnatal stay in hospital until the blood pressure has been controlled for 24-48 hours, depending on the severity of symptoms and blood pressure readings.
- Anti-hypertensive drugs (drugs to lower the blood pressure) should not be stopped without close medical supervision, and this should usually be done gradually.
- If the high blood pressure does not eventually disappear after the birth, the condition will be diagnosed as non-pregnancy hypertension, which will require treatment to control cardiovascular problems in later life.
How should pre-eclampsia be managed after delivery?
All women should have their blood pressure checked soon after the birth.
The condition of some women with pre-eclampsia will deteriorate soon after delivery and midwives and doctors monitor affected women very carefully.
Approximately a third of women with pre-eclampsia and pregnancy induced hypertension will continue to have high blood pressure after the birth or have a recurrence of high blood pressure within a week of birth, and 5-6% of women who develop pre-eclampsia will develop it in the postnatal period for the first time.
You may be asked to stay in hospital until your blood pressure can be maintained below 150/100mmHg, and this could take a few days.
Will I get high blood pressure in my next pregnancy?
If you had high blood pressure before you became pregnant or had blood pressure problems in this pregnancy, you have a greater risk of similar complications in future pregnancies.
This risk depends on how severe your problem was and how many weeks pregnant you were when the high blood pressure started.
- If you developed high blood pressure in your previous pregnancy the chance in future of developing blood pressure problems in your next pregnancy is 1 in 5 (20%)
- If you developed pre-eclampsia after 37 weeks, there is about a one in ten to one in twenty (5-10%) chance that it will happen again.
- If you developed pre-eclampsia between 34 and 37 weeks, there is about a 1 in 4 (25%) chance that it will happen again.
- If you developed pre-eclampsia between 28 and 34 weeks, there is about a 1 in in 3 (33%) chance that it will happen again.
- If you developed pre-eclampsia before 28 weeks, there is about a 1 in 3 to 1 in 2 (33-50%) chance that it will happen again.
Pre-eclampsia may occur at a similar time or later in your next pregnancy, but it is likely to be less severe than the first time.
If you get pregnant again, please make sure you see your GP as soon as possible. Starting low-dose aspirin (150mg daily) from 12 weeks’ gestation in your next pregnancy can significantly reduce the risk of high blood pressure and pre-eclampsia happening again.
Will I have high blood pressure when I am older?
If you have had high blood pressure in pregnancy you have an increased risk of having certain health problems later in life, especially if your baby was delivered before 37 weeks. You may be able to reduce the risk of these conditions if you have regular check-ups and make healthy lifestyle choices.
The problems related to long-term high blood pressure (Chronic Hypertension) include:
- Venous thromboembolism – blood clots that can move to the lungs.
- Cardiovascular disease – problems with your heart and your blood vessels like palpitations, heart attacks or angina.
- Cerebrovascular disease – problems with the blood vessels in your brain such as stroke or mini-stroke and dementia.
- Renal disease – problems with your kidneys that could lead to needing dialysis.
- Retinal disease – problems with your eyes that can lead to poor vision or blindness.
Staying Healthy
What can I do now?
Make sure your blood pressure is well controlled. This will reduce your chances of complications now and in the future.
Make sure you:
- Follow the plan for blood pressure checks with your midwife, health visitor and GP.
- Take your medications as advised.
- If you have any questions or you run out of medicines, speak to your GP.
What can I do long-term?
There are lots of things you can do to try and stay healthy. Talk to your GP if you need help with any of these:
- Regular exercise - for example, 20 minutes fast walking a day.
- Eat a healthy, balanced diet - your GP can give you advice.
- Do not drink too much alcohol (less than 14 units a week is advised).
- Keep to a healthy weight for your height - your GP or health visitor can give advice.
- Do not smoke cigarettes or take recreational drugs – for help on quitting see your GP for a local programme.
- If you are diabetic, make sure you keep your blood sugars within your targets.
- Have your blood pressure and cholesterol checked at least once a year by your GP.
More information
Action on Pre-eclampsia: www.action-on-pre-eclampsia.org.uk Helpline: 01386 761 848
NHS Choices for information on healthy eating and exercise following childbirth: https://www.nhs.uk/conditions/pregnancy-and-baby/keeping-fit-and-healthy/
NICE Guideline Hypertension in Pregnancy, available from https://www.nice.org.uk/guidance/qs35Leaflet
-
Corticosteroid treatment in Hyperemesis Gravidarum
The leaflet is detailed below, or you can download the 'Corticosteroid treatment in Hyperemesis Gravidarum' leaflet in PDF.
What is Hyperemesis Gravidarum?
Nausea and vomiting in pregnancy are very common, affecting up to 80% of pregnant women.
Hyperemesis gravidarum (HG) is a severe form of nausea and vomiting during pregnancy; this is less common, affecting 1-3 in every 100 pregnant women. This type of nausea and vomiting in pregnancy is diagnosed by your healthcare practitioner when you have significant dehydration (feeling dry mouthed, very thirsty, drowsy or you have dark urine) and weight loss.
Some women with this condition need to be admitted to hospital for support. This can include fluids through a drip or medications as injections or through a drip as well as nutritional support.
Why does Hyperemesis Gravidarum happen?
Nausea and vomiting in pregnancy and hyperemesis gravidarum are thought to be due to the pregnancy hormone, human chorionic gonadotrophin (hCG). There is no clear reason why some women get it worse than others. It is more likely to occur if you have had it before, you are having twins or triplets or rarely, if you have been diagnosed with a molar pregnancy (where the placenta overgrows and the pregnancy does not form correctly).
Where can I find out more about Hyperemesis Gravidarum?
The team at the women’s are always happy to discuss HG or any concerns you have. We have a leaflet about sickness and vomiting in pregnancy on our website that can be found here.
www.liverpoolwomens.nhs.uk/media/2755/die_2018-192-v2-sickness-vomiting-in-pregnancy.pdf
There is also an excellent online support network through the charity Pregnancy Sickness Support. This can be accessed on the web address below
www.pregnancysicknesssupport.org.uk
We would encourage anyone affected by nausea and vomiting in pregnancy and their families to visit this site as it has a lot of information, advice and support.
What are corticosteroids?
Corticosteroids are strong anti-inflammatory, immunosuppressive and anti-sickness medications. There is increasing evidence that steroids are an effective treatment for hyperemesis gravidarum.
The way they help with anti-sickness is unclear.
Corticosteroids have been used for a long time in pregnancy for other conditions such as acute asthma, inflammatory bowel disease and to speed up lung development in babies at risk of premature birth.
At what point should I be treated with corticosteroids for hyperemesis gravidarum?
Your doctor will consider prescribing you a course of corticosteroid treatment after you have tried other anti-sickness medications, and they have not been effective at reducing or stopping your vomiting symptoms. This is a medication that is only started in hospital by the specialist early pregnancy team. Corticosteroids are termed a “third-line” medication which means that you will be prescribed both first- and second-line treatment prior to consideration of this therapy. See example below:
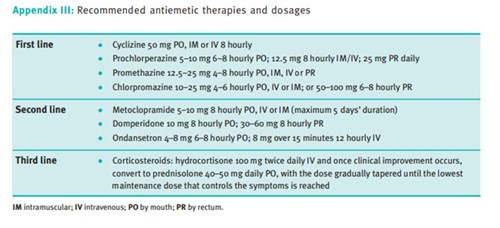
Table 1. Recommended anti-sickness therapies (RCOG GTG 69)
Benefits of corticosteroid use in hyperemesis gravidarum
There is good evidence that corticosteroids can dramatically improve the symptoms of severe hyperemesis gravidarum that have not responded to other anti-sickness therapies.
How will I take corticosteroids?
Corticosteroids are usually started while you are in hospital. They will be commenced intravenously (through the vein) at a high dose. When you feel better, they will be given as oral tablets and gradually reduced over several weeks (Table 1) until they are stopped altogether or continued at a low dose.
Are there any side effects?
Side effects of corticosteroids are uncommon - your doctor should prescribe the lowest effective dose for the shortest time possible.
Examples of side effects include some disturbance of mood, developing ulceration of the gastric tract (your stomach and bowel) and muscle breakdown. Less commonly, changes in your blood pressure, swelling and electrolyte disturbances (the salts in your blood) can occur. With prolonged use they are associated with diabetes, gestational diabetes, and osteoporosis (bone thinning).
Seek medical attention if you experience visual disturbances for example, blurring of your vision.
Are there any reasons I should not be taking corticosteroids?
This medication should not be used if you have a widespread serious infection.
Are corticosteroids safe for me to take during pregnancy?
Corticosteroids are generally safe to take in pregnancy. Only a small amount of corticosteroids used for hyperemesis gravidarum pass through to your baby.
There is some association between taking corticosteroids in pregnancy and cleft lip/palate. Since 2003 no study has proven a significant risk but the rate for cleft lip/palate is believed to be increased from 1.7 to 2.7 per 1,000 babies born to mums who have taken corticosteroids in pregnancy.
It is important to stress that the effects of hyperemesis gravidarum itself on pregnancy can be significant. HG is associated with low birth weights, preterm birth, dehydration and malnutrition for mum, increased risk of blood clots and in some circumstances families having to make the very difficult and heart-breaking decision to end a pregnancy because they cannot continue with the sickness.
Your obstetrician may recommend that you have a test for gestational diabetes during your pregnancy if corticosteroids are taken long-term.
When will I stop taking corticosteroids in my pregnancy?
Most women will stop corticosteroid treatment by 18-20 weeks of pregnancy. 1 in 5 women may require a low dose for the rest of the pregnancy to control nausea and vomiting, sometimes until delivery.
The most important thing when you stop your steroids is that you do it gradually. This is usually done by reducing the dose by 5mg (1 tablet) each week. For some women this causes the nausea and vomiting to return. If this is the case we would advise you to go back to the dose level that stopped your sickness symptoms.
Who will look after me as my pregnancy progresses?
You will be followed up by a consultant in the antenatal clinic. They will advise you further on managing your medications and will arrange growth scans for your baby from 30 weeks.
Further information
Liverpool Women’s Hospital website
There are information leaflets on the website for early pregnancy. Look for the tab for patients, then patient information leaflets. Select gynaecology and you will see and area for early pregnancy. Here are all our specific early pregnancy leaflets. Below is the direct link to the sickness and vomiting in pregnancy leaflet
www.liverpoolwomens.nhs.uk/media/2755/die_2018-192-v2-sickness-vomiting-in-pregnancy.pdf
Pregnancy sickness support
An online charity for women and their families who suffer sickness and vomiting in pregnancy
www.pregnancysicknesssupport.org.uk/get-help/treatments/
Royal college of Obstetricians and Gynaecologists (RCOG)
This is our medical body that produces guidance and support for doctors, nurses and midwives caring for women and their families in pregnancy. They also write information leaflets for women and their families. They have information on pregnancy Sickness (nausea and vomiting of pregnancy and hyperemesis gravidarum) accessible at
https://www.rcog.org.uk/en/patients/patient-leaflets/pregnancy-sickness/
-
Preventing a pressure ulcer during labour and after delivery
The leaflet is detailed below, or you can download the 'Preventing a pressure ulcer during labour and after delivery' leaflet in PDF.
A guide for parents
A pressure ulcer (also known as a bedsore or pressure sore) is an injury to the skin and underlying tissue, caused by prolonged pressure on the skin by anything, but most commonly during delivery, it’s a surface such as a mattress or a medical device such as a urinary catheter.
This can happen to anyone, and women who are in labour are particularly at risk for a number of reasons and changes that happen to women in labour.
Pressure ulcers can affect any part of the body but are most common on bony parts such as coccyx (base of spine), hips, heels and elbows. They can occur in a few hours.
Early signs of a pressure ulcer include:
- Spot of skin becoming discoloured – this may appear red, purple or blue.
- Discoloured patches will not turn white when pressed need to be elevated.
- A patch of skin that feels warm, spongy or hard, or painful.
Later signs of a pressure ulcer include:
- An open wound or blister (category two pressure ulcer)
- A deep wound that reaches the deeper layers of skin (category three)
- A very deep wound that may reach the muscle and bone (category four pressure ulcer)
Preventing pressure ulcers during delivery
People often associate pressure ulcers with the elderly population, however pressure ulcers can occur in anyone at any age who has a prolonged period of immobility, has medical devices attached to them or their sensation is altered due medications, epidurals or anaesthetic.
Skin damage during labour usually occurs in four ways:
- Pressure – as a result of sitting or lying for too long without moving or a device such as a catheter, IV lines, oxygen tubing.
- Shearing/friction – similar to a carpet burn, this can occur when moving around the bed on the bedsheets.
- Moisture – moisture such as amniotic fluid (your waters breaking), urine and sweat can cause moisture damage, giving a ‘chapped’ appearance.
Changing position
Moving and regularly changing your position particularly when you have an epidural is the most important element of pressure relief. The reduced sensation means you don’t feel the prolonged pressure like you normally would. Just a tilt (around 30 degrees should do) or roll to one side helps to relieve the pressure.
Please make sure you are not sat on any uncushioned parts of our delivery beds, folded over sheets or medical device lines.
You should aim to tilt or change your position hourly if you have an epidural or if you’ve had a spinal anaesthetic and your midwife will help to remind you.
You may also be given training and advice about better sitting and lying positions, how you can adjust your sitting and lying positions.
If you have a catheter, make sure you are not sat or lay on the tubing, this should rest above your leg usually on your thigh.
Mattresses and Cushions
If you're particularly at risk of getting pressure ulcers or have an ulcer, your midwife or tissue viability nurse will recommend a specially designed static foam or dynamic mattress or if you’re really at risk you'll need a more sophisticated mattress or bed system, such as a mattress connected to a pump that delivers a constant flow of air into the mattress, but this will after you have delivered your baby.
Your midwife will help you to prevent pressure ulcers by:
Helping or reminding you to change position every hour if you have an epidural or have had a caesarean section until you can move around yourself.
Helping you to get out of bed after 6 hours after your delivery if you have had a caesarean section, ventouse or forceps delivery – even if your catheter is still in.
Removing your catheter as soon as clinically possible after you have delivered your baby. Making sure your catheter is not under your leg or bottom.
Assessing your risk levels when you arrive at the hospital and at regular intervals throughout your stay.
Diet and Nutrition
Eating a healthy, balanced diet that contains enough protein and a good variety of vitamins and minerals can speed up the healing process.
If your diet is poor, you may need to see a dietitian. They can draw up a suitable dietary plan for you.
It's also important to drink plenty of fluids to avoid dehydration, because being dehydrated can slow down the healing process.
Diabetes
If you have diabetes, it’s important that your blood sugar is well controlled – having high blood sugar can increase the chances of having a pressure ulcer or wound infection as this condition slows down the healing process.
In summary
Not every woman in labour will develop a pressure ulcer; however, there are certain procedures and medical devices which can increase your risk. Our midwives on the delivery suite will help and support you to reduce this risk and prevent pressure ulcers.
-
Fetal Growth Clinic: When your baby is smaller than expected
The leaflet is detailed below, or you can download the 'Fetal Growth Clinic' leaflet in PDF.
Why have I been referred to the Fetal Growth Clinic?
You have recently had an ultrasound scan to estimate the weight of your baby. Your baby weighs less than expected when plotted on your customised growth chart. Your customised growth chart is specific for your height, weight and ethnicity to make this assessment more accurate.
How do we monitor the growth of your baby?
Early in pregnancy, your midwife or doctor will identify if you have risk factors for having a small baby, such as; smoking, current or previous problems with raised blood pressure, have had a previous small baby. If this is the case ultrasound scans will be arranged for you during your pregnancy to measure the growth of your baby.
If your pregnancy is assessed to be low-chance for growing a small baby your midwife will measure your bump at every antenatal visit from 24-28 weeks gestation. This measurement will be plotted on your customised growth chart. If, when plotting the measurement on this chart your baby appears smaller than expected, you will be referred for an ultrasound scan.
The measurement of your bump may not be accurate for some women particularly those who are overweight, if your baby is lying in a sideways position and for those with known fibroids in the uterus. For these women ultrasound scans will be arranged to measure the size of your baby.
What happens at my ultrasound scan?
At your ultrasound scan appointment, your baby will have measurements taken of its head, tummy (abdomen) and leg (femur) and from this its weight will be estimated. This weight will be compared against how many weeks pregnant you are (gestation) on your customised growth chart. You will also have measurements taken of the blood flow (Doppler) in your baby’s umbilical cord, brain and sometimes the liver. On your first visit you will also likely have the blood flow in your vessels that supply your womb with blood (uterine arteries) measured.
What do we mean when we say your baby is small?
A baby which is small for gestational age (SGA) measures in the lowest 10% of average ultrasound scans, below the bottom black line (10th centile) on the growth chart. 9/10 babies would measure larger at the same point in pregnancy. However, most of these babies are healthy during pregnancy, delivery and afterwards are like babies who are not SGA. These babies usually continue to put on a good amount of weight throughout the pregnancy and have no problems with the blood flow measurements on the scans. However, in some cases it could be that your baby is not growing as well as they should - this is called fetal growth restriction (FGR). This is often due to the placenta not working as well as it should to support your baby’s growth. These babies are often below the 3rd centile (bottom grey line) and/or have problems with their blood flow measurements. In a small number of cases genetic problems in the baby or infections can cause FGR.
How will my baby and I be monitored during pregnancy?
If your baby is SGA then you will be invited to have an ultrasound scan every 2-3 weeks to monitor your baby’s growth, amount of fluid around them (amniotic fluid volume) and blood flow. This may be in the Fetal Growth Clinic, Main Ultrasound Department or Maternity Assessment Unit.
If your baby has FGR then you will be invited to have more frequent ultrasound scans. After each scan, we will explain the findings and discuss when we need to assess your baby again. In addition to monitoring your baby’s growth and blood flow we sometimes also do a test called a computerised cardiotocography (CTG). This helps us assess the baby’s wellbeing in more detail. It is also important for you to keep seeing your midwife regularly so they can regularly check your blood pressure and test your urine.
What can I do to help?
We want to reassure you that in most cases there is nothing you have done or could have done differently to have changed the situation. It is not because you aren’t eating and drinking enough. We advise all pregnant women to have a healthy, balanced diet and stay active. Smoking can cause problems with the placenta and can cause babies to be small. If you do smoke, stopping or cutting down as much as you can is the most positive thing you can do to help your baby be healthier during pregnancy and after birth. We understand that it can be incredibly difficult, but we can support you to stop, just speak to one of the doctors or midwives.
We will ask you to pay close attention to your baby’s movements, this is very important. If your baby’s movements are less than normal (in strength or frequency) or their usual pattern changes (e.g. moving at night) we want you to come to the hospital to get checked over. Please call Medical Admissions Unit (MAU) on: 0151 702 4413 and they will invite you in. Please don’t leave it until the next day, it is important you come and get checked out when you are concerned.
Will I need to have my baby before my due date?
SGA babies with no other concerns can safely be delivered between 38 - 39 weeks. It is safe to aim for a vaginal birth and we recommend ‘starting off’ labour early (an induction of labour) if you have not already gone into labour by then. If your baby is very small, but with normal blood flows, we may suggest for you to have your baby between 37-38 weeks. If there are concerns with the blood flow to your baby from the placenta we will explain when we think the safest time to deliver your baby is. We may suggest a caesarean section if we have concerns your baby may not cope with labour contractions and may give you steroids to help prepare baby’s lungs for birth.
If it is likely your baby will need specialist care from our neonatal team after birth, we will ask the neonatal doctors to talk to you to allow you to ask questions and offer you a tour of our Neonatal Unit before birth.
How can being SGA affect my baby?
How your baby is after delivery is linked to how early they are born, how small they are and whether there are any other complications. The neonatal team will decide whether your baby needs to be admitted to the neonatal unit. If your baby does need admission, you will be able to be with them as much as you want. Your baby will get the best possible care and support. It isn’t possible to say before delivery what exactly your baby will need and how long your baby will need to stay in the neonatal unit, this is different for each baby. The team will assess how they are coping and will regularly discuss their progress with you and plan when they are ready to go home. Generally, babies born at later gestations tend to need less specialist care and need to be kept in hospital for shorter amounts of time. SGA babies also tend to need less care than FGR babies. However, we will not send a baby home unless the team responsible for both you and your baby’s care feel it is safe to do so.
Being born SGA can make it harder for your baby to feed well, maintain a normal body temperature and blood sugar levels. Most SGA healthy babies do very well but may need a little bit of extra care initially. The midwife looking after your baby will ensure that your baby gets the best monitoring after birth.
In rare cases, your baby may have FGR identified early in the pregnancy, which in some cases may be so severe as to prevent your baby being born alive or increase the chance of baby not surviving after birth. We understand that some of these discussions can be very difficult, and we will provide close support. Babies with severe early-onset FGR can have a very difficult time on the neonatal unit and have long-term health concerns such as cerebral palsy or learning difficulties and may have special educational needs
It is not possible to predict if your child will have any of these complications when in the womb or soon after birth and long term follow up by GP or paediatrician is required. The goal of your team will normally be to delay delivery for as long as is safe to do so as all the complications mentioned are reduced by being born later in the pregnancy.
How will this affect future pregnancies?
Having an SGA baby may increase your chances of having another SGA baby in the future. Overall, the chance of a future SGA baby is probably about one in three, and if it does occur, it tends to follow a similar pattern.
In the next pregnancy after a baby with SGA you will be closely monitored with additional scans. If your baby was diagnosed with FGR you will be offered aspirin in future pregnancies to reduce the chance of this happening again. A healthy lifestyle, optimising your body weight for height and stopping smoking may reduce this risk even further.
What to do if you have any questions or concerns
If you have any questions, please contact the Fetal Medicine Unit (0151 702 4072) we will do our best to answer them. If you are concerned about your baby’s movements or if you experience any bleeding, abdominal pain or concern your waters have gone please call MAU on 0151 702 4413.
-
Low Pregnancy Associated Plasma Protein-A (PAPP-A)
The leaflet is detailed below, or you can download 'PAPP-A' leaflet in PDF.
You have been found to have low Pregnancy Associated Plasma Protein-A (PAPP-A). This is measured as part of your combined antenatal screening blood test.
What is PAPP-A?
Pregnancy-associated plasma protein A (PAPP-A) is a hormone produced by the placenta. Low levels of PAPP-A are defined as less than 0.415 MoM. MoM stands for multiple of the median, or average of everyone’s results. A MoM of 1.00 is average; higher than 1.00 is above average; and lower than 1.00 is below average.
What does low PAPP-A mean?
Low PAPP – A is not uncommon and most babies having low PAPP-A during pregnancy, will be born at the expected time and have a normal birth weight. However, some studies have shown low levels of PAPP-A may be associated with;
- A lower birth weight baby (due to the placenta not working as well)
- Having an early birth (preterm, before 37 weeks)
- An increased chance of developing pre-eclampsia
What happens next?
National guidelines suggest that extra scans should be considered to monitor the growth of babies when a low PAPP-A level has been found. Therefore, we would like to offer you a uterine artery doppler scan between 22-24 weeks which will check the blood flow to the placenta. This is an additional scan to your 20-week anomaly scan. We will also arrange for you to have growth scans at 32, 35 and 38 weeks gestation. If these scans identify any issues, the Fetal Medicine Team will put a plan in place with you.
What can I do to help?
We recommend that you take a daily dose of aspirin 150mg, every evening throughout your pregnancy. There is evidence that taking low dose aspirin once a day can help increase the function and blood flow of your placenta. Liverpool Women’s Hospital routinely requests your GP to provide you with a prescription for aspirin. However, it can also be purchased at your local pharmacy.
It is also important that you keep all your routine community midwife appointments, so the health and wellbeing of you and your baby can be monitored throughout your pregnancy. Monitoring your baby’s movements is also an effective way to check your baby’s wellbeing. If your baby’s movements concern you; slow down, change pattern or stop, you must contact the Maternity Assessment Unit immediately.

As smoking can affect the placenta and growth of the baby, we also recommend all pregnant women stop smoking. You can speak to your midwife for referral to our smoking cessation midwife who can provide you with help and support, including the offer of nicotine replacement therapies.
Who can I speak with if I need further information?
If you have any questions you can contact:
Antenatal Screening Office – 0151 702 4106 / 0151 708 9988 (ext 1083)
Screening Team Mobile – 07971 527 341
Maternity Assessment Unit – 0151 702 4413
Fetal Medicine Unit – 0151 702 4072
Plase see QR code for information on baby’s movements; Tommy’s Fetal Movements leaflet- Baby movements in pregnancy | Tommy's (tommys.org)
-
Intrauterine contraception (IUC) insertion at the time of Caesarean birth
The leaflet is detailed below, or you can download the 'Intrauterine contraception (IUC) insertion at the time of Caesarean birth' leaflet in PDF.
This leaflet is for individuals considering the insertion of intrauterine contraception (IUC) at the time of Caesarean birth
Contraception after having a baby
Pregnancy is possible as soon as three weeks after having a baby. Every person differs as to when they might feel ready or comfortable to have sex again after having a baby, and you should not feel pressured or worry about this. Nevertheless, many unplanned pregnancies do occur in the months after having a baby. Even if you would like more children, it is recommended to space pregnancies out by at least 12 months to allow yourself to recover and improve the chances of a healthy future pregnancy. Contraception comes in many forms and is a way to prevent or delay pregnancy.
Intrauterine contraception at caesarean birth
Intrauterine contraception (IUC), previously known as a ‘coil’, is a safe and effective method of contraception. It is easy to have this fitted at the time of a caesarean birth. IUC is a small, flexible, plastic device. It is inserted through the opening in the uterus (womb), after the placenta (afterbirth) has been removed.
There are two main types:
- Progestogen (hormonal) intrauterine system (IUS)
- Copper (non-hormonal) intrauterine device (IUD)
Image of IUC fitted inside the uterus (womb):
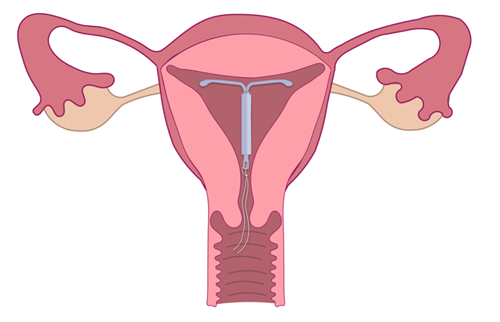
Hormonal intrauterine contraception (also known as intrauterine system or IUS)
- A small plastic device that releases the hormone progestogen.
- This hormone thickens the mucus at the cervix (neck of the womb) to stop sperm entering the uterus and thins the lining of the uterus so an egg cannot implant.
- In some women, it also stops the ovaries from releasing an egg (ovulation), but most women will continue to ovulate.
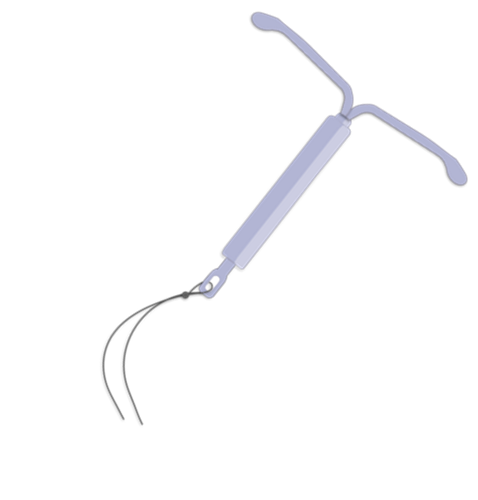
The copper intrauterine contraception (also known as intrauterine device or IUD)
- A small device made from plastic and copper.
- Copper prevents sperm and egg from surviving. It may also stop a fertilised egg from implanting into the womb.
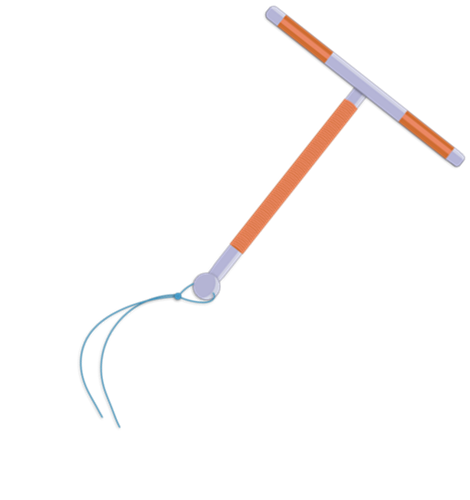
Why might you choose to have an IUC at Caesarean birth?
- The procedure is very safe and quick. It is painless as you will already have an anaesthetic (medication to prevent pain) for the birth.
- It provides protection from pregnancy straight away and for a long time after - 6 to 10 years, depending on device.
- IUC is You do not need to remember to take it every day like a pill, for example.
- IUC contraception is safe when breastfeeding.
- IUC is easy to remove and fertility returns straight away.
Is there anything else I need to know?
There are some specific risks of having intrauterine contraception fitted at the time of Caesarean birth:
Long threads
As your uterus returns to its pre-pregnancy size, you may notice the threads protruding out of the vagina. If this happens the threads can be easily trimmed by a doctor or nurse. If the threads are long, please be careful not to pull the IUD/IUS.
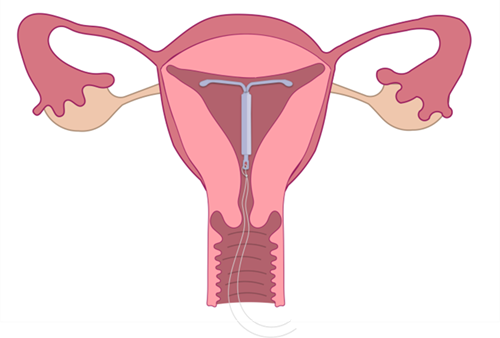
Non-Visible threads
The threads of the device usually come out of the cervix (the neck of the womb) and sit at the top of the vagina so you would not normally feel them. This is to make checking or removing the device more straightforward.
When the IUC is fitted at the time of Caesarean birth the threads can sometimes stay within the uterus. The IUC will still work in the same way and can still be removed with a straightforward procedure, but this will need to be done in Axess sexual health (contact details are provided further on in the leaflet).
Expulsion (falling out)
There is a 1 in 20 chance of the device coming out of the uterus after insertion. This may be slightly higher if having IUC fitted at the time of Caesarean birth. One study found a one in 12.5 chance of expulsion.
The following risks are present whether IUC is inserted at the time of Caesarean birth or inserted at a later date:
Injury or trauma
There is a less than 1 in 1000 chance of perforation (putting a hole) in the uterus at the time of insertion.
Infection
There is a less than 1 in 100 chance of infection in the first few weeks following insertion of the IUC.
Pregnancy risk
The risk of getting pregnancy whilst the IUC is in place is very low. However, if a pregnancy does occur there is a small risk of this being an ectopic pregnancy (a pregnancy that develops outside of the uterus). It is important to seek medical attention if you find yourself pregnant with an IUC in place, or if you have any unusual pain in your lower abdomen.
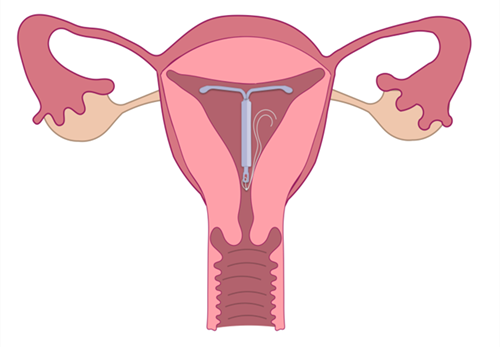
What happens after the device is fitted?
We will arrange for you to have an ultrasound scan and a check to see if the threads need trimming around 6 weeks after the device was fitted. This will be at Axess at The Beat sexual health clinic in Liverpool. You will be contacted with an appointment time.
If before your appointment you experience any problems or have any concerns about your IUC, you can contact Axess at The Beat sexual health clinic on: 0300 323 1300 Option 4
When the IUC is placed inside the womb at caesarean birth, there may be a higher chance that the threads will not be seen at the check-up visit. This does not affect how the IUC works and most can be removed easily when required.
What do I need to do if I want IUC inserted at the time of my Caesarean birth?
If you want to know more or would like to have an IUC inserted at the time of your Caesarean birth, please let your midwife or doctor know. They will be able to assess if this is a safe option for you and make any necessary arrangements.
I’m not sure – where can I find out more information?
You can have a look at the Axess sexual health website where you will find more information or ask your doctor or midwife for a leaflet.
Hormonal IUS:
https://www.axess.clinic/information/contraception/hormonal-coil-ius/
Copper IUD:
https://www.axess.clinic/information/contraception/non-hormonal-coil-iud/
More information on contraception choices after having a baby can be found at the following websites:
- NHS website
https://www.nhs.uk/conditions/contraception/?tabname=getting-started
- Contraception Choices
If you have any further questions you can speak to your midwife or doctor (GP or maternity doctor) or contact the dedicated team at Axess sexual health using the details below.
Axess at the Beat, Liverpool City Centre
Phone number: 0300 323 1300 and select Option 4.
-
Contraception After Having a Baby
The leaflet is detailed below, or you can download the 'Contraception After Having a Baby' leaflet in PDF.
This leaflet is for individuals considering their contraceptive choices after having a baby
Contraception is used to prevent pregnancy. This may be the last thing on your mind after having your baby, however many unplanned pregnancies occur in the first few months after childbirth, so even if you are not interested in sex right now, it is best to be prepared.
When can I start having sex again?
You can have sex as soon as you and your partner both want to. Everyone is different, so don't feel pressured or worry about it if you don’t feel ready right now. Having a baby causes many physical and emotional changes for both partners and it may take some time before you feel comfortable or ready to have sex.
When can I start using contraception?
It is best to have started contraception by three weeks after your baby is born (but the sooner the better). Waiting at least 1 year after giving birth before getting pregnant again can help you have a healthier pregnancy and birth, reducing the risk of complications such as an early birth or a very small baby.
Your midwife will discuss contraception with you during one of your antenatal visits so that you can have your contraception ready to start as soon as you have your baby. Staff in the hospital or community, your GP or local sexual health clinic are all places you can get advice about contraception.
What methods are available to me?
Read this leaflet to get more detailed information about each method and a better idea of what might suit you.
Contraceptive Options
There are many safe and effective options, and contraceptive choice depends on your personal preference as well as your medical history, whether you are breastfeeding and future fertility plans.
Contraceptive effectiveness largely depends on whether it is taken correctly. The most effective methods are those that don’t require a person to remember to take it regularly.
These methods are commonly referred to as “long-acting methods of contraception” (or “LARC”) and include:
- The hormonal intrauterine system (IUS)
- Copper intrauterine device (IUD)
- The contraceptive implant
- The contraceptive injection
There are other methods available that are effective providing they are taken correctly:
- The progestogen only pill (1 hormone)
- The combined contraceptive pill, patch or vaginal ring (2 hormones)
- Condoms
Each method is discussed individually in this leaflet, with typical and perfect effectiveness figures provided.
- ‘Perfect’ use refers to if a method is taken correctly.
- ‘Typical’ use refers to the average use taking into account mistakes (such as a missed pill) interfering illnesses or medication.
If a method is quoted as 99% effective, this means that out of 100 women having sex using this method for one year, one woman will get pregnant.
Contraception and breastfeeding
When you are breastfeeding, most contraceptive options do not affect your baby or your supply of milk. Combined contraceptive methods are the only method that should be slightly delayed.
Breastfeeding is not a reliable method of contraception. However, you are less likely to get pregnant if:
- Your baby is less than six months old and
- Your periods have not come back and
- You are fully breastfeeding day and night with no bottle feeds at all.
If you have problems with breastfeeding or milk supply, you should contact the your midwife or health visitor for advice.
Hormonal intrauterine device (LNG-IUD)
The hormonal intrauterine device (LNG-IUD) is a small, T-shaped device placed into your uterus (womb). It releases a small amount of hormone, called progestogen, which prevents sperm from getting through the cervix into the uterus and meeting an egg. It may give you lighter or no periods.
Advantages
- Lasts for up to 5-6 years
- It can be fitted at the same time as a Caesarean birth
- More than 99% effective (both perfect and typical use)
- It can be removed easily, with a quick return to fertility
- Very low dose of a safe hormone
- Periods/bleeding will most likely be lighter (or bleeding might stop altogether)
- Suitable for breastfeeding women
- You don’t have to remember to take a pill every day.
Disadvantages
- Possible irregular bleeding, which usually settles after a few months
- Must be inserted by a clinician.
When can I start using this after I have my baby?
The hormonal IUS can be fitted either at the time of a planned Caesarean birth or four weeks after a vaginal or Caesarean birth. You can discuss this with your midwife or doctor.

Copper (hormone free) intrauterine contraceptive device (Cu-IUD)
The copper IUD is a small, T-shaped device that is placed in your uterus (womb) and alters the way sperm move. This prevents them from fertilising an egg. This IUD has a small amount of natural, safe copper. It’s 100% hormone free and doesn’t alter periods.
Advantages
- Lasts for up to 5 or 10 years (depending on the type of Copper IUD)
- It can be fitted at the same time as a Caesarean birth
- More than 99% effective
- It can be removed easily with a quick return to fertility
- No hormones
- You don’t have to remember to take a pill every day
- Continued regular periods, which some women prefer
- Suitable for breastfeeding women.
Disadvantages
- Possible heavier, crampier periods
- Must be inserted by a clinician.
When can I start using this after I have my baby?
The copper IUD can be fitted either at the time of a planned Caesarean birth or four weeks after a vaginal or Caesarean birth. You can discuss this with your midwife or doctor.
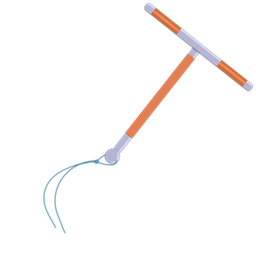
Implant
The implant is a tiny rod, about the size of a matchstick that is inserted into the upper arm. The implant releases a hormone called progestogen that prevents your ovaries from releasing eggs and thickens your cervical mucus, which helps to block sperm from getting to the egg in the first place.
Advantages
- It can be inserted as soon as you have your baby, either before leaving the hospital or after discharge by a GP or local sexual health clinic.
- Lasts for three years
- More than 99% effective
- Easy to remove with a quick return to fertility
- May have lighter or no periods
- Suitable for breast feeding women
- You don’t have to remember to take a pill every day.
Disadvantages
- Possible irregular periods (or no periods).
When can I start using this after I have my baby?
You can use this immediately after having your baby. It can be inserted in the hospital before going home or in a local sexual health clinic or GP.

Contraceptive Injection
The contraceptive injection contains progestogen, a hormone that prevents your ovaries from releasing eggs. It also thickens your cervical mucus, which helps to block sperm from getting to the egg in the first place.
Advantages
- It can be given as soon as you have had your baby, either before leaving the hospital or after discharge by a GP or local sexual health clinic.
- Lasts for 3 months
- 99% effective if injections with perfect use, 94% effective with typical use
- May have lighter or no periods
- It is suitable for breastfeeding women.
Disadvantages
- Must see a health professional every three months for the injection (unless you choose the injection that you can give to yourself)
- Possible delay in return to fertility on stopping
- Possible irregular periods.
When can I start using this after I have my baby?
You can use this immediately after having your baby. It can be given in the hospital before going home.

Progestogen only pills
These pills contain only one hormone, progestogen. This method suits women who want to take pills but who cannot have oestrogen. The pills are taken every day. There are two kinds of progestogen only pill: the traditional ones that thicken cervical mucus and stop sperm reaching the egg and the newer ones that keep the ovaries from releasing an egg.
Advantages
- The pills can be started as soon as you have had your baby- you can be prescribed these in hospital or after discharge by a GP or local sexual health clinic.
- 99% effective with perfect use, 91% effective with ‘typical’ use
- Reversible after stopping
- Suitable for breastfeeding women
- Safe for women who cannot have oestrogen
- May have no bleeding.
Disadvantages
- May have irregular bleeding
- Must remember to take at the same time each day.
When can I start using these after I have my baby?
You can use these immediately, if you want to. Your midwife can give you a supply of pills before leaving hospital

Combined hormonal contraception
These methods contain two hormones, oestrogen, and progestogen, that prevent your ovaries from releasing an egg. Usually this is a pill that you take at the same time every day. There are lots of different kinds of pills on the market. There are also patches or vaginal rings which work just like the pill.
Advantages for these methods
- 99% if taken perfectly, 91% effective with ‘typical’ use
- Shorter, lighter and less painful periods
- Reversible after stopping
- May help with acne.
Disadvantages
- May have irregular bleeding, usually improves over time
- Must use the method correctly
- Some women cannot take oestrogen for health reasons.
When can I start using these after I have my baby?
If you are breast feeding you cannot use a combined hormonal method until 6 weeks after you have had your baby. If you are not breast feeding, then you may be able to start combined hormonal contraception at 3 weeks after you have your baby, but some women may need to wait until 6 weeks after delivery due to health reasons. You can use another method in the meantime.


Female sterilisation
This involves blocking the fallopian tubes so that sperm cannot get through to meet an egg. There are different ways of doing this. You will need to have it done in hospital. If you are thinking about having female sterilisation you should speak to your doctor as soon as possible so they can advise you about what your options are. Remember that the intrauterine methods (hormone IUS and copper IUCD) and implant mentioned in this leaflet are at least as effective as female sterilisation.
Advantages
- Permanent
- More than 99% effective
- No change in periods.
Disadvantages
- Higher failure rate if done during caesarean section
- Irreversible
- Must be certain you never want another pregnancy
- Surgical procedure
- Might require general anaesthetic
- Risk of complications.
When can I start using this after I have my baby?
You will normally be advised to wait until your youngest child is a year old before you have the operation. If you have a planned caesarean section, it may be possible to have this done at the same time.
Male sterilisation – vasectomy
This involves blocking the tubes (vas deferens) that take sperm from the testicles to the penis. It is a quick procedure done under local anaesthetic. To arrange this, you should ask your GP for a referral to the local service that provides this. Male sterilisation is more effective than female sterilisation and a much simpler procedure. Remember that the intrauterine methods (hormone IUS and copper IUCD) and implant mentioned in this leaflet are very effective, reversible methods.
Advantages
- Permanent
- More than 99% effective
- Local anaesthetic.
Disadvantages
- Irreversible
- Surgical procedure
- Risk of complications.
When can I start using this after I have my baby?
You will normally be advised to wait until your youngest child is a year old before you have a vasectomy. Ask your GP for referral when your baby is 6-9 months.
 Barrier methods
Barrier methods“Barrier methods” includes external (male) condoms, internal (female) condoms and diaphragms. These methods are much less effective at preventing pregnancy compared to other methods in this leaflet.
External condoms are most effective when used perfectly. They’re 98% effective at preventing pregnancy with perfect use and 82% effective with typical use. Female condoms are diaphragms are less effective than this.
Advantages
- You only need to use them when you have sex.
- Condoms can help to protect both partners from some sexually transmitted infections (STIs), including HIV.
- There are no serious side effects from using condoms.
Disadvantages – external condoms
- A condom can sometimes slip off or split and are only effective if used correctly from the very start of sex, and if removed correctly.
- They interrupt the flow of sex and sometimes people decide not to use them in the moment.
When can I start using this after I have my baby?
You can use condoms straight away after having a baby.
You can start using a diaphragm from 6 weeks after childbirth. If you used a diaphragm or cap before getting pregnant, go to your GP or local sexual health clinic to ensure it still fits correctly.
Emergency contraception
If you have unprotected sex in the first 3 weeks after having your baby, you will not need emergency contraception. If you have any sex after the first 21 days without using reliable contraception, then you could get pregnant.
Speak to your GP, local pharmacy or sexual health clinic for more advice and to obtain emergency contraception.
A note on the withdrawal method
The withdrawal method or “pulling out” is probably better than doing nothing.
However, the risk of it not working is about 22% which means that about 1 in every 5 (or 22 per 100) women relying on withdrawal will become pregnant. Even with perfect use, there is still a risk of sperm entering the vagina before ejaculation.
The NHS does not recommend this as a reliable way to prevent pregnancy.
Services
At the Liverpool Women’s Hospital
You can speak to your midwife or doctor before you have your baby or afterwards before you go home from hospital.
Once you have gone home your community midwife can also provide support and advice.
GP
Your local GP practice can provide contraception, and many GP practices provide intrauterine contraception (IUS or IUD) or the implant or can refer onto another local GP practice.
Sexual health clinics
There are many sexual health clinics in Liverpool and the surrounding areas that can provide contraception. Information for these based on where you live is listed below:
Liverpool, Knowsley, Cheshire East, Warrington & Halton
Axess sexual health. Use the website or telephone number to find your local service:
https://www.axess.clinic/find-service/
0300 323 1300
St Helen’s
St Helen’s Sexual Health
https://getiton.org.uk/Pages/default.aspx
01744 646473
Southport, Bootle, Maghull, Netherton
Sefton Sexual Health
https://www.seftonsexualhealth.nhs.uk
01695 656550
The Wirral
Sexual health Wirral
https://www.sexualhealthwirral.nhs.uk
0300 123 5474
Lancashire & West Lancashire
https://lancashiresexualhealth.nhs.uk/find-nearest-centre/
0300 1234 154
For Wigan & Leigh
Find a clinic - Spectrum SHS (spectrum-sexualhealth.org.uk)
01942 483188
-
Birth Place Decisions
The leaflet is detailed below, or you can download 'Birth Place Decisions' leaflet in PDF.
Information to help you plan where to give birth
Maternity care aims to offer you personalised care. It is important that you are aware of the birth options available to you so that you can make an informed decision. Your Midwife or Obstetrician (Doctor) can help you to understand your options and you are welcome to use this document as a guide for discussion. We want to provide you with accurate information so that you can make an informed decision about your place of birth.
At Liverpool Womens, we encourage women and staff to use the ‘BRAIN Tool’ to support birth choice discussions. You can find further information about this on the back page of this leaflet.

This guide is intended to support you to plan where to have your baby. The information is based upon the best available evidence, including a large study of 64,500 women (Birthplace Study, 2011) and National Institute for Health and Care Excellence ‘Intrapartum care for healthy women and babies (NICE CG190, 2022). The leaflet offers information to help you make an informed decision. You can alter your plans at any stage as your pregnancy progresses, or if you change your mind. The evidence shows that giving birth in the UK is generally very safe.
For most women giving birth is generally very safe. Whether it is your first or subsequent pregnancy, you will be supported to have your baby in the place you feel most comfortable and you your support partner may remain with you throughout your labour and birth. Research shows that for low-risk women you have a greater chance of vaginal birth when you deliver your baby on a Midwifery-Led Unit, or at home, compared to an Obstetric Unit (Delivery Suite).
A small number of babies will have unexpected medical problems during or after birth. Some are less serious and not permanent, and a very small number are serious and result in permanent injury. The risk is higher for babies born at home, but it is still a very small number (9 for every 1000 births) and our midwives are trained to manage emergency situations to minimise risk.
For women who are at increased risk of complications, we will recommend that you have your baby on the main Delivery Suite. This is to provide better access to a wider medical and clinical team, with more specialised equipment. However, if you would like to consider birthing at home, or on the midwifery-led unit please let us know as early as possible after your 20 week scan.
There are three options where you can give birth at the Liverpool Women’s Hospital. You may choose to give birth:
- You may have had a baby before and did not experience any complications.
- You are expecting one baby in this pregnancy.
- Your baby is head down.
- Birth takes place between 37- 42 weeks.
- No complications have developed before or during labour.
Birth settings available at Liverpool Women’s
Home birth
The Home Birth Team are a group of experienced midwives, dedicated to providing midwifery care throughout the pregnancy journey to women who are considering birthing at home.
The Home Birth Team provide a 24/7 service, giving you access to a known midwife throughout your pregnancy, birth and after your baby is born.
If you are considering a home birth and would like to find out more information, please contact the Home Birth Team by texting 07976835735 or by email at home.birth@lwh.nhs.uk

Midwifery Led Unit (MLU)
MLU is an ideal place for women who could have their baby at home but wish to be closer to medical support. Research shows that women who are at low risk of complications, who deliver in a home environment are less likely to have intervention associated with labour and birth, and the outcome for the baby is no different compared with obstetric units.
Birthing rooms on MLU are designed to create a ‘home from home’ environment.

Midwives will support you to be mobile in labour and adopt upright positions to achieve optimum conditions for natural birth.
Hydrotherapy, aromatherapy and pharmacological forms of pain relief (gas and air, tablets and / or injections) are available on the MLU. Should you request an epidural, this will involve being transferred to the main Delivery Suite.

Delivery Suite
Our Delivery Suite (Obstetric unit) provides specialist care for women in labour and immediately after birth. We have more equipment available to monitor you and your baby.
It is recommended to birth your baby on the Delivery Suite if you are:
- Under 37 weeks pregnant.
- Offered induction of labour.
- Have a medical condition requiring specialist care.
- Having twins or triplets.
- Are experiencing bleeding in pregnancy.
- Baby is breech (bottom down instead of head down)
- Waters have broken for more than 24 hours.
- Have an infection that could be passed to your baby.
The rooms are larger with more specialist equipment ready for use if needed. All rooms have en-suite facilities.

The Delivery Suite provides 24/7 specialist care with a range of available specialists:
- Midwives
- Obstetricians
- Neonatologists
- Anaesthetists
What happens If I have to transfer into hospital from home?
If you have chosen to have a homebirth, then your midwife will complete a risk assessment, ensuring your home is accessible to ambulances in the instance that you would require a transfer to hospital.
When the ambulance arrives, the crew will assess your condition so that the transfer can happen quickly and safely. In an emergency, you may be taken to the nearest maternity unit and not your preferred hospital. This will happen if it is the safest option for both you and your baby. Your personal situation will be categorised into either of the following:
Category One: An emergency with life threatening consequences.
Category Two: Transfer is required for care that is urgent, but not life-threatening. For example: delay in labour, pain relief, maternal request, perineal suturing.
Please note, there is a distinction between the ambulance response time and the transfer time from your home to the hospital. The previous months average response time for both category 1 and category 2 are available on NHS England Website and will be discussed with you should you wish to birth outside of the hospital setting.
Your personal transfer time will be a combination of the response time, plus the estimated time travel from your home to the hospital.
What to do if you have not been given a choice.
There is clear NICE guidance that women who are at low risk of complications should have an opportunity to choose where to birth their baby.
Your community midwife will complete a birth assessment with you at your 36-week antenatal appointment. However, you are welcome to talk about labour and birth at any time. If you are at a higher risk of complications, it may be suggested to have your baby on the Delivery suite. However, you are welcome to attend a further appointment with a Consultant Midwife or Obstetrician to consider birthing on the MLU or at home.
At Liverpool Women’s Hospital, Doctors and Midwives use the BRAIN tool to support shared decision-making and we invite you to also consider this tool when considering your options.
BRAIN Tool
B – Benefits: What are the benefits of making this decision / taking this course of action?
R – Risks: What are the risks associated with this decision / action?
A – Alternatives: Are there alternatives? If so, what are they?
I – Intuition: How do I feel? What is my ‘gut’ telling me?
N – Nothing: What if I decide to do nothing / Wait and see? What happens next?
Further Information and Resources
This leaflet is intended to support your decision about where to have your baby. Please take time to talk to your birthing partner and midwife about your needs and wishes. We want to support you to achieve a positive experience of birth.
The following resources will also help you to read around this important decision a little more:
NICE Clinical Guideline 190 (Updates Dec 2022)
Recommendations | Intrapartum care for healthy women and babies | Guidance | NICE
Birthplace Study (2011)
Birthplace in England Research Programme | SHEER | NPEU (ox.ac.uk)
NHS Choices (Your choice where to have your baby).
www.nhs.uk/Pages/HomePage.aspx
Which? Birth Choices Website
-
Monochorionic Diamniotic (MCDA) - Liverpool Multiple Pregnancy Clinic (LMPC)
The leaflet is detailed below or you can download the 'Monochorionic Diamniotic (MCDA)' leaflet in PDF.
The Liverpool Multiple Pregnancy Clinic
Congratulations on your pregnancy, and welcome to the Liverpool Multiple Pregnancy Clinic (LMPC).
Liverpool Women’s Hospital hosts one of only a few dedicated multiple pregnancy clinics in the UK. This service has been designed to provide all of the antenatal care that you should need throughout your pregnancy.
You will see a Specialist Multiple Pregnancy Midwife who will talk you through the plan of care for your pregnancy and answer any questions that you may have.
Your scans will be performed in the Fetal Medicine Unit (FMU) by a team of specialist doctors and consultants.
Your Multiple Pregnancy Team
- Professor Asma Khalil
- Dr Andrew Sharp, Consultant
- Dr Ben Choo, Consultant
- Dr Borna Poljak, Specialist Doctor
- Anne Rhodes, Midwife Sonographer
- Jennifer Robinson, Specialist Multiple Pregnancy Midwife
- Claire Coonan, Specialist Multiple Pregnancy Midwife
Your specialist midwives and medical team would like to welcome you to the wonderful world of multiples.
We love it and we hope you will too. However, we also know that this can be a very confusing and frightening time. Jen and Claire live in this world and encourage you to feel free to talk to them about any questions you may have.
What is multiple pregnancy, and why do I need extra appointments?
The aim of this booklet is to introduce the different types of multiple pregnancy, and explore the known risks. This helps us follow a detailed pathway to minimise these risks to you and your unborn children. The appointments for review and scanning times, can be longer than in other pregnancies, but we will keep you informed regarding any delays.
We also want to empower you to make decisions about your antenatal classes, delivery, and pain relief, plus where to seek additional support if required.
Multiple pregnancy means carrying more than one baby (referred to as singleton pregnancy). Most multiple pregnancies are Twins, rather than triplets and quadruplets. Multiple pregnancy is increased by fertility treatment, ethnic origin, and the later ages of mums having their children.
Twins can be monozygotic (one fertilised egg splits in two) or dizygotic (two eggs are fertilised). Monozygotic Twins will normally be the same sex. There are generally three types of Twins seen on scan. The three types are:
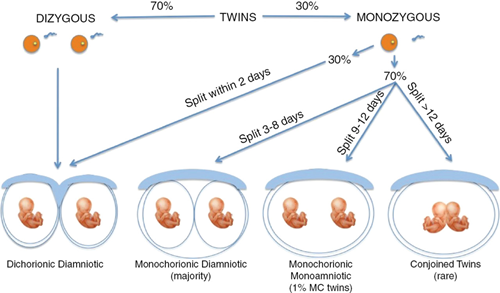
(From Fetal Medicine, RCOG Bidyut Kumar, Zarko Alfirevic)
All non-identical Twins are DCDA, and roughly one-third of identical Twins are DCDA. The other two-thirds of identical Twins are MCDA, and just 1% of identical Twins are MCMA.
One-third of all Twins will be identical, and two-thirds non-identical
Identical (monozygotic) Twins happen when a single egg is fertilised. The egg then divides in two, creating identical Twins who share the same genes. Identical Twins are always the same sex and they’ll look very alike.
The majority of women who are pregnant with Twins deliver healthy babies, although carrying more than one baby increases the health risks for the mother and the babies. This is of particular importance if the placenta is shared between Twins, as in 70% of identical Twins. The best time to identify the chorionicity (whether the placenta is shared or not) is on your dating scan at 12 weeks of pregnancy. If the scan cannot identify as to whether the placenta is shared or not, you will be monitored as for a monochorionic (shared placenta) pregnancy.
Screening
If you wish to have screening for conditions such as Down’s syndrome- this is still possible. You will be offered a blood test in combination with your dating ultrasound (using measurements from each baby) between 11-14 weeks of pregnancy. This generates a likelihood of a baby having a condition such as Down’s syndrome. Only those deemed high risk (1 in 150 chance) would then be offered more invasive tests to give a final diagnosis.
Private screening tests to detect the babies DNA within a maternal blood sample are non-invasive and accurate screening tests in singleton pregnancies. Unfortunately, they are less accurate in multiple pregnancy and fail to obtain a result 5% of the time.
A member of the LMPC team will be able to discuss this in further detail if required.
What specifically are the doctors and midwives looking for?
Whilst we would like every pregnancy to go perfectly, unfortunately this is not always the case and Twin pregnancies are at greater risk of some complications.
Preeclampsia
Raised blood pressure in pregnancy is linked with multiple pregnancy. If you have other risk factors for preeclampsia, your doctor may wish for you to start on Aspirin 150mg a day, to help reduce the risk. At every appointment your blood pressure and urine is checked to identify preeclampsia. Urine pots can be collected from the desk. If you experience swelling of the face, severe headaches, visual disturbances, or upper abdominal pain, please contact the hospital immediately. These may be signs that you are developing pre-eclampsia and you will need to be assessed by our medical team.
Anaemia
Anaemia is common in multiple pregnancies due to the extra dietary demand on your body. It is important to eat a healthy diet, your midwife will be able to recommend a variety of foods that can help you avoid anaemia during your pregnancy. You will be offered at least two blood tests to detect anaemia to enable treatment at an early stage. Signs of anaemia can be tiredness, shortness of breath, light headedness and looking pale. We may recommend taking iron tablets to minimise the chance of developing anaemia.
Gestational Diabetes
This is a condition when your blood glucose (sugar) is raised during pregnancy. It is more likely to occur when you are having more than one baby, are overweight, older, or have a family history of diabetes. Your midwife will check your urine at every appointment, if there is glucose in your urine on more than one occasion, she may send you for a glucose tolerance test (GTT). If you do develop gestational diabetes you will be managed by our dedicated diabetes team as well as us, it can be successfully managed minimising the risks of complications.
Obstetric Cholestasis
Obstetric cholestasis is a condition, more common in multiple pregnancies, where the normal flow of bile from the liver is restricted. The main symptom is severe itching, especially the palms and soles, as well as tiredness, dark urine and loss of appetite. Please talk to your midwife about any changes or concerns you may have, and she will offer additional tests. If you do develop obstetric cholestasis then you will be put on medication, some women will need to be delivered early as a result of the condition.
Vaginal Bleeding
Bleeding of any sort can be extremely worrying in pregnancy, please contact the hospital if you experience bleeding during your pregnancy.
Preterm Birth
Women expecting Twins or triplets are more likely to delivery preterm
- About 60 in 100 sets of Twins will go into labour before 37 weeks
- About 75 in 100 sets of triplets will go into labour before 35 weeks
- In comparison, only about 10 in 100 women who are pregnant with one baby will give birth before 37 weeks.
Preterm birth may have a relatively minor effect on your babies if it occurs close to 37 weeks, but a much more serious impact if it begins at lower gestations. In light of this we advise that all women have an assessment of their cervical length on vaginal scan at 20 weeks. This is performed separately to the scan looking at your babies’ anatomy. If the cervix is short at this time, then you may be offered treatment to prevent early delivery.
Problems with growth
A difference of up to 25% between the weights of Twins is considered normal. If the difference (discordance) is greater than this, you may be asked to see the medical team for further scans.
Labelling of Twins
We label your babies Twin 1 and Twin 2 from early in the pregnancy. In rare cases because the position of the babies can change it may not be Twin 1 that is delivered first. Please check with your midwife at delivery.
Problems Specific to Monochorionic Twins
Unfortunately, because of the shared placenta in monochorionic twins these pregnancies are at higher risk of complications than dichorionic twins.
Twin-to-Twin Transfusion Syndrome (TTTS)
TTTS occurs in 10-15% of monochorionic twin pregnancies, meaning about 85% of do not develop this condition.
There are abnormal connections between the baby’s blood vessels on the surface of the placenta. This then causes blood to be transferred (shunted) from one twin (the donor) to the other (the recipient).
By donating some of its blood supply to its sibling, the donor has less oxygen in its blood and produces less urine, leading to a small bladder and less fluid around the baby. The recipient has excess fluid and a large bladder.
You will have regular ultrasound scans in pregnancy to screen for TTTS. The diagnosis is made by measuring the amount of fluid around each baby, the size of their bladders, the baby’s weight and the baby’s blood flows (Dopplers).
There are a few warning symptoms to keep an eye out during your pregnancy but often you will have no symptoms at all:
- Sudden weight gain
- Feeling of increased pressure in your tummy
- Feeling like your tummy is tight
If you are diagnosed with TTTS, you and your babies will be monitored very closely. If the TTTS is mild (stage 1) and the babies are stable, you may not need any treatment. You will be regularly monitored and if the situation gets worse, doctors may intervene.
If the TTTS is more advanced, you will be advised about treatment options. If no treatment is performed the outcome for the pregnancy can be very bad. The most effective treatment is Laser Ablation of the blood vessels of the placenta which connect the babies. It involves a needle being inserted into your uterus (womb). More information will be provided with our TTTS leaflet should you develop this condition.
Selective Fetal Growth Restriction (sFGR)
In 10-15% of Monochorionic twin pregnancies the babies do not share the placenta evenly. This means that one baby gets a normal amount of nutrition from its mother whilst the other baby gets less than it needs to grow efficiently.
We monitor the babies growth with ultrasound and will try to gain as much gestation as possible. Sometimes we will need to deliver early to ensure that both babies are born healthy.
Making the most of your pregnancy
Your pregnancy may seem to pass you by in a flash, with all your specialist appointments and preparation in welcoming your new babies. Here at LMPC we feel that it is important to make the most of this short and precious time. It can be stressful having more than one baby and at times it may seem overwhelming. Here are a few tips to help you to enjoy your pregnancy. Try to eat a well-balanced diet. Taking regular exercise can be very beneficial when pregnant even if you’re not used to doing so. It does not have to be going to classes or going the gym, going swimming is a great way to exercise in pregnancy. However, you can go for a walk for free! It is well documented that being at one with nature can boost mental wellbeing and you can do it in any weather and do not need any specialist equipment. It is also recommended to talk to your babies before they are born as it is known to enhance brain development and bonding. Anyone in the family can talk to the babies and about anything at all, it does not have to be children’s stories. If you are struggling with ideas, why not start by reading them this booklet, once you start you will find it becomes easier each time. By the time they are born it will be second nature. It is not advisable for you to smoke, drink alcohol or take non-prescribed drugs during your pregnancy. If you would like help and advice on giving up, please talk to your midwife and she will help.
Antenatal Classes
Our specialist multiple pregnancy midwives run regular antenatal classes designed to give you guidance and answer your questions on pregnancy, birth and looking after your new babies. We also include advice on twin related issues and difficulties, such as breast-feeding two babies (dates available in the clinic).
Labour and delivery
As multiple pregnancies are higher risk for both you and your babies, we advise that you deliver in a consultant led unit. This will mean easier access to doctors for yourself and babies, if required. We advise delivery from 35+0 weeks of pregnancy for triplets, from 36+0 for monochorionic, and from 37+0 weeks if carrying dichorionic Twins.
Giving Birth to Twins
If the presenting Twin is head down (cephalic) we would advise vaginal delivery as there is no evidence that elective caesarean section is any better for mother or babies. The position of the second baby does not affect the chance of a vaginal delivery. Previous caesarean section is not a contraindication to vaginal delivery.
Of those pregnancies where an attempt at vaginal delivery is made approximately 50% will result in caesarean section. In addition, there is a 7% risk of having to deliver the second twin by caesarean section.
If you have not laboured spontaneously, we would advise induction of labour. This will be performed in hospital (see induction of labour leaflet).
If the presenting Twin is breech, we recommend caesarean section unless spontaneous labour has occurred and vaginal delivery is imminent.
Your midwives will discuss a plan for delivery with you at 28 weeks or sooner if needed.
Fetal Monitoring
All Twin pregnancies should be monitored with continuous electronic fetal monitoring, referred to as a CTG, during labour. A clear difference between both babies heartbeat should always be identified on monitoring. A fetal scalp electrode (FSE) may be offered to Twin I to aid in differentiating the babies.
Analgesia
All options for analgesia can be considered during labour and the choice of analgesia is yours. There are some benefits in using epidural analgesia if additional procedures should be required for the delivery of Twin 2. This can be discussed in more detail with your midwives in LMPC.
What do I need to pack for hospital?
As you may require a hospital stay during your pregnancy, we would recommend at around 24 weeks you pack an overnight bag just in case you should need it.
We have prepared a list to help guide you when packing you bag.
For your babies:
- Cotton wool
- Nappies – approximately 8 per day per baby
- Vests – 5-6 per baby
- Baby grows 5-6 per baby
- At least 1 cardigan per baby
- At least 1 hat per baby
- Scratch mitts
- Although the hospital provides blankets and towels, you may like to bring your own
For you:
- Maternity pads
- Breast pads (even if you are not breast feeding)
- Nursing bras + underwear
- Nightie/PJ’s 2-3
- Dressing gown + slippers
- Change of clothes
- Toiletries
- Towel (the hospital does have towels, but they are not very big)
- Flannel
- Hair bands
- Lip balm
- Snacks and drinks
- HOSPITAL NOTES
NICU
Twins are more likely to spend time in a special care baby unit than a singleton. We understand that this can be a worry to parents. Here at Liverpool Women’s, we have a fantastic world Neonatal Unit with highly trained doctors and nurses who all understand the feelings you may experience should one or more of your babies need extra support.
Twins go to our neonatal unit for a variety of reasons and spend different lengths of time there. It is worth noting that if one of your babies needs to go to the unit, it does not mean they will both go, this can be very stressful, but rest assured that your babies bond will not be disturbed and that you can spend time with both your twins together. If either of your babies had to go to the Neonatal unit, it would be a good idea for you to think about giving them breast milk, as this will aid their recovery, your midwife can discuss this further with you at any point.
Postnatal Management
We expect that you will return home, happy and healthy, with your new babies, and postnatal care is the generally the same as for those returning home with one baby. As many multiple pregnancy babies will need to spend some time on the neonatal unit (NICU) this can cause concern and feelings of separation. We advise that you speak to your midwife and neonatal nursing staff for reassurance.
We strongly advise breast feeding as the best form of nutrition your babies can receive in early life. Your midwife and our breastfeeding team can help support you in this.
Research in Multiple Pregnancies
Liverpool Women’s Hospital and LMPC is heavily involved in research and you may be asked to consider taking part. A Midwife or Doctor will discuss suitable research with you and answer any questions you may have. All research is voluntary and you do not need to take part if you do not want to.
Useful Contacts
If you would like further information about multiple pregnancy and birth, you may find the following resources helpful
Useful websites
Twins Trust www.twinstrust.org
NHS Choices www.nhs.uk
National Institute of Clinical Excellence (NICE) www.nice.org.uk
Infant feeding information
Association of Breastfeeding Mothers Tel: 0844 209 0920 www.abm.me.uk
Twins Trust www.twinstrust.org
Financial advice
Social Media
Facebook: Breastfeeding Twins and Triplets UK
-
Dichorionic Diamniotic (DCDA) - Liverpool Multiple Pregnancy Clinic (LMPC)
The leaflet is detailed below or you can download the'Dichorionic Diamniotic (DCDA)' leaflet in PDF.
The Liverpool Multiple Pregnancy Clinic
Congratulations on your pregnancy, and welcome to the Liverpool Multiple Pregnancy Clinic (LMPC).
Liverpool Women’s Hospital hosts one of only a few dedicated multiple pregnancy clinics in the UK. This service has been designed to provide all of the antenatal care that you should need throughout your pregnancy.
You will see a Specialist Multiple Pregnancy Midwife in our multiple pregnancy antenatal clinic (LMPC), who will talk you through the plan of care for your pregnancy and answer any questions that you may have. Most of your scans will be performed in the main ultrasound department (USS).
Your Multiple Pregnancy Team
- Dr Liz Stephenson, Consultant, DCDA Twins lead
- Jennifer Robinson, Specialist Multiple Pregnancy Midwife
- Claire Coonan, Specialist Multiple Pregnancy Midwife
- Elaine Glennon, Ultrasound Lead for Multiple Pregnancy
What is multiple pregnancy, and why do I need extra appointments?
The aim of this booklet is to introduce the different types of multiple pregnancy and explore the known risks. This helps us follow a detailed pathway to minimise these risks to you and your unborn children. The appointments for review and scanning times, can be longer than in other pregnancies, but we will keep you informed regarding any delays.
We also want to empower you to make decisions about your antenatal classes, delivery, and pain relief, plus where to seek additional support if required.
Multiple pregnancy means carrying more than one baby (referred to as singleton pregnancy). Most multiple pregnancies are Twins, rather than triplets and quadruplets. Multiple pregnancy is increased by fertility treatment, ethnic origin, and the later ages of mums having their children.
Twins can be monozygotic (one fertilised egg splits in two) or dizygotic (two eggs are fertilised). Monozygotic Twins will normally be the same sex. There are generally three types of Twins seen on scan. The three types are:
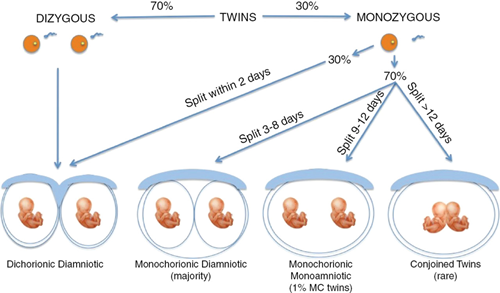
(From Fetal Medicine, RCOG Bidyut Kumar, Zarko Alfirevic)
All non-identical Twins are DCDA, and roughly one-third of identical Twins are DCDA. The other two-thirds of identical Twins are MCDA, and just 1% of identical Twins are MCMA.
One-third of all Twins will be identical, and two-thirds non-identical
Identical (monozygotic) Twins happen when a single egg is fertilised. The egg then divides in two, creating identical Twins who share the same genes. Identical Twins are always the same sex and they’ll look very alike.
The majority of women who are pregnant with Twins deliver healthy babies, although carrying more than one baby increases the health risks for the mother and the babies. This is of particular importance if the placenta is shared between Twins, as in 70% of identical Twins. The best time to identify the chorionicity (whether the placenta is shared or not) is on your dating scan at ~12 weeks of pregnancy. If the scan cannot identify as to whether the placenta is shared or not, you will be monitored as for a monochorionic (shared placenta) pregnancy.
Screening
If you wish to have screening for conditions such as Down’s syndrome- this is still possible. You will be offered a blood test in combination with your dating ultrasound (using measurements from each baby) between 11-14 weeks of pregnancy. This generates a likelihood of a baby having a condition such as Down’s syndrome. Only those deemed high risk (1 in 150 chance) would then be offered more invasive tests to give a final diagnosis.
Private screening tests to detect the babies DNA within a maternal blood sample are non-invasive and accurate screening tests in singleton pregnancies. Unfortunately, they are less accurate in multiple pregnancy and fail to obtain a result 5% of the time.
A member of the LMPC team will be able to discuss this in further detail if required.
What specifically are the doctors and midwives looking for?
Whilst we would like every pregnancy to go perfectly, unfortunately this is not always the case and Twin pregnancies are at greater risk of some complications.
Preeclampsia
Raised blood pressure in pregnancy is linked with multiple pregnancy. If you have other risk factors for preeclampsia, your doctor may wish for you to start on Aspirin 150mg a day, to help reduce the risk. At every appointment your blood pressure and urine is checked to identify preeclampsia. Urine pots can be collected from the desk. If you experience swelling of the face, severe headaches, visual disturbances, or upper abdominal pain, please contact the hospital immediately. These may be signs that you are developing pre-eclampsia and you will need to be assessed by our medical team.
Anaemia
Anaemia is common in multiple pregnancies due to the extra dietary demand on your body. It is important to eat a healthy diet, your midwife will be able to recommend a variety of foods that can help you avoid anaemia during your pregnancy. You will be offered at least two blood tests to detect anaemia to enable treatment at an early stage. Signs of anaemia can be tiredness, shortness of breath, light headedness and looking pale. We may recommend taking iron tablets to minimise the chance of developing anaemia.
Gestational Diabetes
This is a condition when your blood glucose (sugar) is raised during pregnancy. It is more likely to occur when you are having more than one baby, are overweight, older, or have a family history of diabetes. Your midwife will check your urine at every appointment, if there is glucose in your urine on more than one occasion, she may send you for a glucose tolerance test (GTT). If you do develop gestational diabetes, you will be managed by our dedicated diabetes team as well as us, it can be successfully managed minimising the risks of complications.
Obstetric Cholestasis
Obstetric cholestasis is a condition, more common in multiple pregnancies, where the normal flow of bile from the liver is restricted. The main symptom is severe itching, especially the palms and soles, as well as tiredness, dark urine and loss of appetite. Please talk to your midwife about any changes or concerns you may have, and she will offer additional tests. If you do develop obstetric cholestasis then you will be put on medication, some women will need to be delivered early as a result of the condition.
Vaginal Bleeding
Bleeding of any sort can be extremely worrying in pregnancy, please contact the hospital if you experience bleeding during your pregnancy.
Preterm Birth
Women expecting Twins or triplets are more likely to delivery preterm
- About 60 in 100 sets of Twins will go into labour before 37 weeks
- About 75 in 100 sets of triplets will go into labour before 35 weeks
- In comparison, only about 10 in 100 women who are pregnant with one baby will give birth before 37 weeks.
Preterm birth may have a relatively minor effect on your babies if it occurs close to 37 weeks, but a much more serious impact if it begins at lower gestations. In light of this we advise that all women have an assessment of their cervical length on vaginal scan at 20 weeks. This is performed separately to the scan looking at your babies’ anatomy. If the cervix is short at this time, then you may be offered treatment to prevent early delivery.
Problems with growth
A difference of up to 25% between the weights of Twins is considered normal. If the difference (discordance) is greater than this, you may be asked to see the medical team for further scans.
Labelling of Twins
We label your babies Twin 1 and Twin 2 from early in the pregnancy. In rare cases because the position of the babies can change it may not be Twin 1 that is delivered first. Please check with your midwife at delivery.
Making the most of your pregnancy
Your pregnancy may seem to pass you by in a flash, with all your specialist appointments and preparation in welcoming your new babies. Here at LMPC we feel that it is important to make the most of this short and precious time. It can be stressful having more than one baby and at times it may seem overwhelming. Here are a few tips to help you to enjoy your pregnancy. Try to eat a well-balanced diet. Taking regular exercise can be very beneficial when pregnant even if you’re not used to doing so. It does not have to be going to classes or going to the gym, going swimming is a great way to exercise in pregnancy. However, you can go for a walk for free! It is well documented that being at one with nature can boost mental wellbeing and you can do it in any weather and do not need any specialist equipment. It is also recommended to talk to your babies before they are born as it is known to enhance brain development and bonding. Anyone in the family can talk to the babies and about anything at all, it does not have to be children’s stories. If you are struggling with ideas, why not start by reading them this booklet, once you start you will find it becomes easier each time. By the time they are born it will be second nature. It is not advisable for you to smoke, drink alcohol or take non-prescribed drugs during your pregnancy. If you would like help and advice on giving up please talk to your midwife and she will help.
Antenatal Classes
Our specialist multiple pregnancy midwives run regular antenatal classes designed to give you guidance and answer your questions on pregnancy, birth and looking after your new babies. We also include advice on twin related issues and difficulties, such as breast-feeding two babies (dates available in the clinic).
Labour and delivery
As multiple pregnancies are higher risk for both you and your babies, we advise that you deliver in a consultant led unit. This will mean easier access to doctors for yourself and babies, if required. We advise delivery from 35+0 weeks of pregnancy for triplets, from 36+0 for monochorionic, and from 37+0 weeks if carrying dichorionic Twins.
Giving Birth to Twins
If the presenting Twin is head down (cephalic) we would advise vaginal delivery as there is no evidence that elective caesarean section is any better for mother or babies. The position of the second baby does not affect the chance of a vaginal delivery. Previous caesarean section is not a contraindication to vaginal delivery.
Of those pregnancies where an attempt at vaginal delivery is made approximately 50% will result in caesarean section. In addition, there is a 5% risk of having to deliver the second twin by caesarean section.
If you have not laboured spontaneously, we would advise induction of labour. This will be performed in hospital (see induction of labour leaflet).
If the presenting Twin is breech, we recommend caesarean section unless spontaneous labour has occurred and vaginal delivery is imminent.
Your midwives will discuss a plan for delivery with you at 28 weeks or sooner if needed.
Fetal Monitoring
All Twin pregnancies should be monitored with continuous electronic fetal monitoring, referred to as a CTG, during labour. A clear difference between both babies heartbeat should always be identified on monitoring. A fetal scalp electrode (FSE) may be offered to Twin I to aid in differentiating the babies.
Analgesia
All options for analgesia can be considered during labour and the choice of analgesia is yours. There are some benefits in using epidural analgesia if additional procedures should be required for the delivery of Twin 2. This can be discussed in more detail with your midwives in LMPC.
What do I need to pack for hospital?
As you may require a hospital stay during your pregnancy, we would recommend at around 24 weeks you pack an overnight bag, just in case you should need it.
We have prepared a list to help guide you when packing you bag.
For your babies:
- Cotton wool
- Nappies – approximately 8 per day per baby
- Vests – 5-6 per baby
- Baby grows 5-6 per baby
- At least 1 cardigan per baby
- At least 1 hat per baby
- Scratch mitts
- Although the hospital provide blankets and towels, you may like to bring your own
For you:
- Maternity pads
- Breast pads (even if you are not breast feeding)
- Nursing bras + underwear
- Nightie/PJ’s 2-3
- Dressing gown + slippers
- Change of clothes
- Toiletries
- Towel (the hospital does have towels, but they are not very big)
- Flannel
- Hair bands
- Lip balm
- Snacks and drinks
- HOSPITAL NOTES
NICU
Twins are more likely to spend time in a special care baby unit than a singleton. We understand that this can be a worry to parents. Here at Liverpool Women’s we have a fantastic Neonatal Unit with highly trained doctors and nurses who all understand the feelings you may experience should one or more of your babies need extra support.
Twins go to our neonatal unit for a variety of reasons and spend different lengths of time there. It is worth noting that if one of your babies needs to go to the unit, it does not mean they will both go, this can be very stressful, but rest assured that your babies bond will not be disturbed and that you can spend time with both your twins together. If either of your babies had to go to the Neonatal unit, it would be a good idea for you to think about giving them breast milk, as this will aid their recovery, your midwife can discuss this further with you at any point.
Postnatal Management
We expect that you will return home, happy and healthy, with your new babies, and postnatal care is the generally the same as for those returning home with one baby. As many multiple pregnancy babies will need to spend some time on the neonatal unit (NICU) this can cause concern and feelings of separation. We advise that you speak to your midwife and neonatal nursing staff for reassurance.
We strongly advise breast feeding as the best form of nutrition your babies can receive in early life. Your midwife and our breastfeeding team can help support you in this.
Research in Multiple Pregnancies
Liverpool Women’s Hospital and LMPC is heavily involved in research and you may be asked to consider taking part. A Midwife or Doctor will discuss suitable research with you and answer any questions you may have. All research is voluntary and you do not need to take part if you do not want to.
Useful Contacts
If you would like further information about multiple pregnancy and birth, you may find the following resources helpful
Useful websites
Twins Trust www.twinstrust.org
NHS Choices www.nhs.uk
National Institute of Clinical Excellence (NICE) www.nice.org.uk
Infant feeding information
Association of Breastfeeding Mothers Tel: 0844 209 0920 www.abm.me.uk
Twins Trust www.twinstrust.org
Financial advice
Social Media
Facebook: Breastfeeding Twins and Triplets UK
Your DCDA Pregnancy Pathway
Gestation
Purpose of Visit
Location
11-13
Dating scan
Record chorionicity and fetal labelling
Offer combined screening for Down’s syndrome
Reassess risks as now known multiple pregnancy
Give aspirin if appropriate (150mg at night)
Explain and document plan of care
Booking Clinic
16
Antenatal assessment
(Quadruple test if required)
Check Booking Blood Results
Cervical length scan
LMPC
20
Antenatal assessment
Anomaly scan
LMPC
USS
24
Antenatal assessment
Full Blood Count
Discuss preterm labour
Issue MatB1 form
Growth scan
LMPC
USS
28
Antenatal assessment
FBC and Antibody screening
(Anti D if required)
Discuss infant feeding
Discuss Timing and Mode of delivery
Health Visitor Referral
Growth scan
LMPC
USS
32
Antenatal assessment
Birth Plan
Growth scan
LMPC
USS
34
Antenatal assessment
LMPC
36
Antenatal assessment
Arrange steroids if required
Growth scan
LMPC
USS
37 onward
Weekly CTG and consultant review if declines delivery
-
Induction of Labour
The leaflet is detailed below, or you can download the 'Induction of Labour' leaflet in PDF.
Information on what happens next for those who find themselves booking in for induction of labour.
Useful numbers:
Community Midwife: 0151 708 9988 extension: 4177
Maternity assessment room : 0151 702 4413.
Induction of labour ward : 0151 708 9988 – extension : 1426
Induction of labour co-ordinator: 0151 708 9988 ask for Bleep number 103
This leaflet explains what induction of labour is, why it may be needed, what the risks and benefits are and what to expect if you need to have an induction.
What is Induction of labour (IOL)
In some pregnancies labour starts naturally between 37 and 42 weeks, leading to the birth of your baby. Induction of labour is a process designed to start labour. At Liverpool Women’s Hospital nearly half of women need Induction of labour. This is for the following reasons:
Why might I be offered induction of labour?
Induction of labour will be offered if you and the team caring for you agree because it will benefit you or your baby’s/babies’ health.
IOL is usually recommended in the following circumstances:
- Prolonged pregnancy: After 41 weeks, there is evidence to that stillbirth rates starts to slightly increase:

For this reason, we will offer IOL at 41 weeks (NICE [NG207], 2021)
We will offer you induction of labour at 41 weeks as evidence shows an improvement in outcome for both mothers and babies:

It has been found that induction after 39 weeks but before 41 weeks does not increase your chances of having an instrumental or caesarean section.
- Black, Asian minority ethnic groups and women from poor socio-economic background are known to be at increased risk of still birth. MBRRACE (2020)

Induction of labour to those with additional risks related to ethnicity and / or deprived socio-economic background, will be discussed. Other risk factors which will be discussed with you for possible IOL include:
- Pre-labour rupture of membranes: It is safest to offer IOL as soon as possible because if labour does not start 24 hours after your waters break, there is an increased risk of infection to both you and your baby.
- Over 40 years of age
- Overweight with Body Mass Index of over 35
- Medical reasons: If there are any medical problems in your pregnancy which can affect the health of you or your baby an induction of labour will be discussed with you.
Can labour be encouraged to start naturally?
Yes. A ‘membrane sweep’ is the first step to try and encourage labour to start and it is recommended prior to induction. This can be done by a midwife or a doctor at home, at an antenatal appointment or in hospital. It can reduce the need for other induction methods. A membrane sweep can be offered from 38 weeks if your baby is in the right position.
If you are offered IOL for a medical reason, or if we know that your baby is likely to need admission to the neonatal unit, the Doctor caring for you will discuss this with you and advise on the timing of your sweep. An additional sweep can be offered after 72 hours if labour does not start.
Membrane sweeping involves a vaginal examination whereby your midwife places a finger inside your cervix (also known as the neck of your womb) and makes a circular, sweeping movement to separate the membranes (or waters) from the cervix.

Are there any side effects from having a membrane sweep?
A sweep may cause some discomfort and sometimes slight bleeding. A sweep will not cause harm to you, or your baby and it does not increase your chances of infection. If you are concerned about any blood loss, we have a 24-hour telephone triage that you can access for help and advice (See contact details on page 1). After a sweep, we will offer to listen to your baby’s heartbeat and remind you to continue to make sure your baby is still active, and you are happy with your baby’s movements.
What preparations do I need to make before coming in for my IOL?
We advise you to plan for your induction to take anywhere from 1 to 3 days. This is because whilst we know that each individual’s body will respond slightly differently, and you will be offered the right care for you depending on how your body responds to the induction process. Bringing with you books, magazines, snacks, drinks can help. We will need to prioritise women accordingly to their clinical need and the clinical need of their baby. This means that sometimes you may have a delay in either starting or continuing your IOL journey. We will keep you informed of any delays encountered but please bear in mind that induction can be a lengthy process.
What about my birth partner during induction of labour?
Your birth partner may remain with you during the whole process of induction. However, it may be helpful for them to get some rest prior to active labour which is likely to be at least 24 hours into the process. There will be a recliner chair provided at your bedside for their comfort. Unfortunately, we do not have facilities for partners to wash or shower in the hospital and we cannot provide free meals. You may decide that it is more comfortable for your partner to return home during this early stage of induction. If you start having labour pains in the night you are welcome to ring your birth partner to come and support you. In the meantime, your midwife will check both you and the baby and provide any pain relief you may require.
Can I decide not to be induced?
Yes, it is your choice to decline induction. If you decide against being induced, we may offer you additional checks for you and your baby. A plan will be put in place for the remainder of your pregnancy. This will depend on the reasons for IOL being offered and any other factors which might impact your individual situation. Monitoring and using scans do not help predict or avoid problems that might happen suddenly and none of these tests can accurately predict whether your baby is more or less likely to have a stillbirth in the future but can help to tell you how your baby is at the time of the scan or test.
What happens on the day of my induction?
Before arriving on the day, we ask that you ring first, as sometimes if there is not a bed available straight away, we will take a contact number and telephone you later in the day. Occasionally, we may have to postpone your induction until the following day. In this instance we will offer to provide a full assessment to make sure we keep you and your baby safe.
On arrival for induction
On arrival, you will be welcomed by a member of staff and shown to the induction of labour suite. The midwife caring for you will explain what will happen and you will be shown the information video and asked to sign a consent form if you have not already signed when attending the maternity assessment unit of the postdates clinic. There will be time for you to ask questions that you or your partner may have. The wellbeing of both you and your baby will be checked. This will involve taking your blood pressure, pulse, temperature, feeling the position of the baby (we may use a small ultrasound scan machine) and monitoring the baby’s heartbeat.
You will need to have an internal vaginal examination so that the midwife can assess the neck of the womb (cervix). In pregnancy, the cervix is about 3cm long and quite firm. Before we can start the active part of your induction, the cervix must change so that it feels thin and soft (sometimes called ripening). The cervix is ready for labour when it is thin and soft. We score the cervix on how ready it is for labour. This is called a Bishops Score.

Induction of labour is a medical intervention which aims to start labour. Induction is a “stepped” approach.
The first step is to ripen the cervix (neck of the womb)
The second step is to release the bag of waters around your baby. (often called “breaking the water”)
If you are not contracting regularly the next step is to begin a hormone drip to stimulate your uterus to contract.
The ways in which your labour is induced – First step
Pharmacological (Hormone drugs) or mechanical methods of induction

Pharmacological (Hormonal) Methods of Induction
Propess pessary:
A vaginal examination is needed to place prostaglandin in the form of a pessary close to the neck of the womb.

The pessary will release a small amount of the hormone each hour into the cervix to encourage it to soften and thin. The pessary will stay in place for 24 hours and we will monitor both you and the baby every 6 hours during this time. We will ask that you inform your midwife if:
- You start to have any pains
- Your waters break
- You have any bleeding
- You are concerned that your baby isn’t moving around normally.
During this first 24 hours, you are welcome to move around off the ward and we advise that you eat and drink regularly. This will help provide you with the energy and hydration required the following day for labour.
If the pessary falls out, please let your midwife know.
Occasionally, the cervix takes less time to ripen and the pessary can be removed earlier. If this happens, we will transfer you to Delivery Suite at the next available time so that you can continue with your induction.
A very small number of those undertaking induction will have very frequent contractions and will need to have the Propess removed before 24 hours. This is called hyperstimulation and has the potential to cause adverse effects for you and your baby. You may also require another medication called Terbutaline, given as an injection, to stop contractions.
Prostin gel:
Prostin gel is a prostaglandin gel which is sometimes used when your membranes have ruptured (“waters have gone”) and your cervix remains “unfavourable”. Meaning not soft or effaced.

Prostin Gel is inserted into your vaginal and around your cervix with the aim of softening and effacing the cervix. Its effects are noted after 6 hours.
Prostin Gel can also be used when you have already had the propess suppository in place for 24 hours and your cervix remains unfavourable, and we are unable to break your waters.
Mechanical (Non-Pharmacological) Method of Induction
Cooks Balloon or Foley Catheter – cervical ripening balloon (CRB)
There is a choice to have a non-pharmaceutical induction of labour and sometimes this is recommended. This is usually because there is a history of a previous birth by caesarean section, previous history of surgery on your uterus or sometimes if you have had 4 or more babies born. This will be discussed with you prior to attending for your induction with your consultant obstetrician or midwife.
What is Induction of labour with a CRB? Induction of labour (IOL) is a process used to safely start labour artificially. On admission the balloon is inserted into the cervical canal during an internal examination by the Doctor or Midwife.
There are 2 types of cervical ripening balloons. The Cook’s catheter and the Foley’s catheter. When the Cook’s catheter is used the first of the two balloons (balloon 1) is inflated with a safe liquid called ‘normal saline’ on the uterine side of the cervix and the second (balloon 2) is then inflated in the vaginal side of the cervix. Similarly, when the Foley’s catheter is inserted into the cervical canal during vaginal examination, once in place the balloon will be inflated the uterine side of the cervix. See image below.

The two balloons od the Cook’s catheter or the singular balloon of the Foley’s catheter then adapt to the contour of the cervical canal to minimise discomfort. When the CRB is removed, the cervix will be assessed for dilatation (opening of the cervix) and based on the findings a plan will be made with you regarding the next stage of the induction of labour.
The CRB is made to naturally and gradually dilate the cervix and help start labour. Ripening and dilation works by the balloon’s or balloons’ gentle and constant pressure. This allows pressure from the balloon to ripen the cervix.
As the CRB does NOT contain any medication, it reduces the risk of side effects. Once inserted the CRB will usually stay there for 12-18 hours. It can be easily removed should it need to be taken out before this time.
What are the benefits of the CRB?
The CRB safely softens and opens the cervix without the use of medications, and therefore reduces potential side effects. The silicone balloon adapts to the individual shape of the cervical canal. The balloon is easily inserted and removed.
What happens 12 hours after the CRB is inserted? The CRB will be deflated before being removed. Another internal assessment will be undertaken to assess if your waters can be broken. When a delivery bed becomes available you will be transferred for your waters to be broken. Another internal examination maybe required by a midwife or doctor if your waters cannot be broken, and the findings and plan of care will be discussed with you. You may at this time, be offered the Prostin Gel or a caesarean section following a discussion between you and a doctor.
Breaking your waters – Amniotomy – Second Step
Once your cervix is thin and soft enough, we will start the active part of your labour. This will involve transferring you to Delivery Suite, where you will have your own room and midwife. Breaking your waters will encourage your body to produce a hormone called oxytocin. This will help to bring on stronger contractions that will dilate the cervix. To have your waters broken, you will need to have a vaginal examination and a slim hook will be used to make a hole in the bag of waters. This will not harm your baby, but it maybe uncomfortable for you.

Oxytocin hormone drip may be started if you have not started with any contractions or there are no signs that your cervix has started to dilate. If you have already had a baby following a vaginal birth, it may be appropriate to allow 2-4 hours to see if labour establishes, depending on your wishes.
Oxytocin is a hormone which aids contractions which will be commenced after your waters have been broken. It is given through a drip and carefully regulated to make sure you have the right frequency of contractions until the birth of your baby. The drip can be turned up or down depending on how your body responds. Breaking the waters and the hormone drip takes place on Delivery Suite where you will receive one to one care by a midwife. It is important that we have continuous monitoring of your baby’s heartbeat during this phase of the induction. The pattern of your baby’s heartbeat over a long period of time gives a reliable reflection of how well your baby is coping with labour.
Unfortunately, there are times when this transfer may need to be delayed if the hospital is very busy. We are not always able to provide you with a timeframe for transferring to Delivery Suite, which we understand can be upsetting. If a delay in transfer is likely we will continue to provide care and support on the Induction Suite. The decision on when we can transfer you to Delivery suite to have your waters broken and hormone drip started will be the decision of the Delivery Suite Co-ordinator. This will be when she is certain that one to one care can be provided for you and your baby. This is essential to keep you and your baby safe.
Going home with the pessary – Outpatient IOL.
There are some situations where we would be happy for you to return home after you have attended for the initial monitoring and had the pessary (Propess) inserted or CRB inserted. Outpatient IOL can be considered for women:
- Who are over their due date (Up to 41 weeks and 6 days).
- BMI equal to or less than 40.
- Less than 40 years of age.
- Live within a 12 mile radius of the hospital.
- Pelvic girdle pain (PGP) or symphysis pubic dysfunction (SPD)
- Gestational diabetes (providing no medication has been used in the pregnancy to control blood sugar)
- Previous complications with the birth (heavy bleeding during the last birth for example)
- Once the midwife has given Propess you will be able to return home for 24 hours. If you have had the CRB inserted you wil be able to return home for 12 hours. At the end of this time you return to Induction Suite, Propess or CRB is removed, and you wait with us for a place on Delivery Suite for the next part of the process.
Please return to Induction Suite at any time over the 24 hours if:
- You are contracting frequently
- You have pain that is not controlled with paracetamol
- You have concerns about baby’s movements
- You have any bleeding
- You think your waters have broken.
- If you are having an Outpatient induction and labour starts following Propess, you will probably be suitable for birth on our Midwifery Led Unit following a discussion with a consultant obstetrician or senior doctor.

What are the benefits of IOL?
You have some predictability of when your baby is likely to be born (1-3 days after the date planned for your IOL).
We only offer IOL if we feel that it is safer for either the health of yourself or your baby.
IOL often results in a vaginal birth which means that your recovery period is likely to be quicker than the recovery period for caesarean section.
Vaginal birth increase you chance of future vaginal deliveries.
What are the risks of IOL?
We know that induction of labour is often more painful than spontaneous birth. As a result of this women are found to be more likely to have an epidural once in established labour. Women who have an epidural are slightly more likely to need help birthing their baby. This may be a ventouse or forceps birth.
Occasionally, you can contract too often during the IOL process (this is called tachysystole). This may cause changes to your baby’s heartrate pattern (hyperstimulation) or make it difficult for you to cope with the pain. We sometimes offer a small injection to slow the contractions down in these circumstances.
Sometimes, even with regular contractions your cervix does not dilate. The only option to birth your baby in these circumstances would be to offer you a caesarean section.
Usually, reactions from the pessary are very minor, but sometimes women can experience vaginal soreness.
Analgesia or pain relief during the induction of labour process
Speak to your midwives for more information about your options.
Whilst in the induction of labour area you have several options:
Many people like to start with:
- Distraction techniques, aromatherapy, birth ball and moving around
- Water (There is a bath and showers available to you in the induction areas)
- Tens
- Paracetamol tablets
- Dihydrocodeine tablets

Once you have moved to the labour ward area to continue with the next step of your induction you have other pain relief options available to you:

While in the Induction Suite we can give
- Paracetamol and dihydrocodeine tablets 4-6 hourly for pain relief. Please ask the midwife looking after you for pain relief instead of taking it yourself as we need to monitor the amount of medication you receive as well as your pain levels.
- Diamorphine, Entonox (gas and air) and epidural are available on Delivery Suite.
Please visit www.labourpains.com and look for the pain relief comparison card for more details.
Labour Pains - Information on pain relief choices during labour

-
Parvovirus B19 Infection (Slapped Cheek Disease) in Pregnancy
The leaflet is detailed below, or you can download 'Parvovirus B19 Infection' leaflet in PDF.
What is parvovirus B19 infection and why is it important?
Parvovirus B19 infection is also known as slapped cheek disease, fifth disease or erythema infectiosum.
It is a viral infection that mainly affects school-age children, therefore mothers with young children are particularly at risk of exposure to the infection as well as women working with children (e.g. teachers, childcare workers).
Every 3-4 years there is a seasonal outbreak in the UK peaking during the late winter and early spring months.
Parvovirus B19 usually causes a mild and self-limiting disease in healthy individuals that is followed by lifelong immunity.
Over a half (50-70%) of pregnant women will be immune to parvovirus infection already.
However, if contracted during the pregnancy, it can have a significant impact on the baby.
There is no vaccine or preventative treatment available therefore pregnant women are not routinely screened for past parvovirus infection.
How does the Parvovirus B19 infection spread?
Infection is usually passed by airborne respiratory droplets (coughing and sneezing) from person to person directly or by touching contaminated objects and then touching your face.
The infection usually occurs 14-21 days after the exposure to the virus.
How can the infection be prevented?
To reduce the risk of parvovirus B19 infection you should avoid close contact with people who are unwell, wash your hands regularly and avoid touching your face with unwashed hands.
What are the symptoms of Parvovirus B19 infection?
Symptoms may include feeling unwell, mild fever, headache, runny nose, sore throat, nausea and abdominal pain.
In children ‘slapped cheek’ rash that the disease was named after appears about 7-10 days later as red areas on both cheeks followed by body rash a few days later. The rash is not painful or itchy. One day after the rash appears the child is not infectious anymore.
In adults the rash is less common, and majority will have mild symptoms (if any). Apart from flu-like symptoms described above, commonly reported symptom in adults is joint pain.
What if I have suspected infection or was in contact with a person infected with Parvovirus B19?
Significant contact with an infected person is defined as being in the same room for 15 minutes or more or having face-to-face contact with the person for any length of time.
If you think you’ve been in significant contact with a person with suspected or confirmed Parvovirus B19 infection, contact your midwife or the hospital without delay.
Your midwife will arrange testing of your blood sample that was taken at the time of your booking appointment to determine if you are already immune to Parvovirus B19.
This will help us determine if any further steps are required. If you are immune, no further follow-up is needed as you have antibodies that protect you from the infection. If you are not immune, you are at risk of contracting the infection and we will arrange another blood test screen for infection.
If we do not have your booking blood sample, we will arrange a blood test urgently to find out if you are immune or if you currently have parvovirus infection.
The test results should be available within 3 working days, once requested. You should be contacted with the result as soon as they are received by the hospital. If you do not hear back, it is strongly advised that you contact your midwife or Liverpool Women’s Hospital Antenatal Clinic.
Please avoid contact with other pregnant women and other people at risk of complications (immunocompromised – e.g. receiving chemotherapy, have organ transplant, HIV positive) until you are found to be immune to infection or infection is excluded.
What if I have confirmed Parvovirus B19 infection in pregnancy?
If the blood tests show that you have the infection you will be referred to our Fetal Medicine Unit where your baby will be closely monitored by ultrasound scans.
The monitoring usually starts within 4 weeks of maternal infection and the purpose is to look for any signs of anaemia in the baby (see below).
Please avoid contact with other pregnant women and other people at risk of complications until you are no longer infectious.
Make sure you get enough rest, stay hydrated and take paracetamol for symptom relief (fever, headache, painful joints).
If you have concerns with fetal movements contact Maternity Assessment Unit (Tel. 0151 702 4413) for advice as soon as possible.
What effects does it have on the pregnancy?
It is unusual (occurring in less than 5% of pregnancies) to have a parvovirus B19 infection for the first time in pregnancy.
Complications for the baby usually occur 3-5 weeks after the start of mother’s infection.
In majority of women (70%) the infection will not be transferred through the placenta to the baby and there will be no complications.
Parvovirus B19 is not known to cause birth defects. However, if the infection is passed from the mother to the baby (30% cases of parvovirus in pregnancy) it may cause the baby to become anaemic. 3-11% of these babies can develop hydrops (excess water build up in body cavities).
Because of severe anaemia and/or hydrops, parvovirus infection can cause miscarriage or stillbirth. If infection happens before 20 weeks of gestation, the risk of pregnancy loss is about 7%. The risk of complications is very low if infection is acquired after 20 weeks (<1%), especially in the third trimester.
Intrauterine blood transfusion is a treatment option for severe anaemia that can be done from around 16 weeks, and it involves giving blood to the baby before birth. Majority of the babies will not need treatment and anaemia will resolve spontaneously. If the treatment is required, all the details will be discussed with you in Fetal Medicine Unit.
References:
https://www.gov.uk/guidance/parvovirus-b19
https://cks.nice.org.uk/topics/parvovirus-b19-infection/
https://patient.info/doctor/parvovirus-infection
-
Having a Caesarean Section
The leaflet is detailed below, or you can download the 'Having a Caesarean Section' leaflet in PDF.
What is a caesarean section?
A caesarean section is the delivery of your baby through a cut to your tummy (abdomen) and womb (uterus) in a situation where the anticipated risks of vaginal delivery are greater than caesarean section.
There are two types of caesarean section: Planned and Emergency.
A Planned Caesarean Section is sometimes called an Elective Caesarean Section.
An Emergency Caesarean Section is performed if any complications occur before or during labour.
Common reasons for a planned (elective) caesarean section.
Medical History / Conditions
Occasionally, there may be a medical reason or condition that would cause your Doctor to recommend a caesarean birth for you. These are rare, and they would be discussed with you during your pregnancy.
Malpresentation
Your baby needs to be in a position that will ensure that they will pass safely through the pelvis and birth canal. If the baby is lying in a different position, for example; feet, shoulder, brow or limbs coming first, your baby will not be able to come through your pelvis as safely.
Placenta Praevia
Occasionally, the placenta may be low down and cover the neck of the womb. This can sometimes cause bleeding in pregnancy. Placenta praevia is measured by scan:
- If the placenta is less than 2cm away from the opening of your womb you are likely to be advised to have a caesarean section.
- If the edge of the placenta is more than 2cm away from the opening of your womb then you have a better chance of having a vaginal birth and this would be discussed with you.
Previous Caesarean Section
If you have had a previous caesarean section, it does not necessarily mean that you would be advised to have another. If there were complications during or after your surgery last time, or if there has been less than 6 months between your pregnancies, a further caesarean birth may be recommended.
Maternal Request
Sometimes, if there has been a previous difficult birth, you may wish to choose the option of elective caesarean section for subsequent pregnancies.
There are times when women for a variety of reasons choose to have a planned caesarean birth with their first baby.
This choice is supported at Liverpool Women’s Hospital and you will be offered a separate antenatal appointment to discuss this in more detail.
What are the benefits of caesarean birth?
Caesarean sections largely offer a planned and predictable birth which may offer greater physical or psychological safety depending on your own unique circumstances.
What are the risks of caesarean birth?
Caesarean section is a major operation which carries possible risks to both you and your baby. There are typically more risks associated with caesarean section than vaginal birth.
There are more risks associated with an emergency caesarean, than planned (elective) caesarean. Listed are some of the possible risks:
- Chance of heavy bleeding either during or after the surgery.
- A higher risk of needing a blood transfusion, compared to vaginal birth.
- A small risk of hysterectomy.
- A 6% risk of getting an infection.
- A 5% risk of being readmitted after you have gone home. This is most often due to concerns with bleeding and / or infection.
- There is a very small chance of returning to theatre if there are ongoing concerns.
- A small risk of blood clots that may require daily injections in the early postnatal period.
- A small risk that the structures surrounding the womb can be cut or injured (bladder, bowel, ureters, blood vessels) during the caesarean.
- There is a small risk that your baby can experience a cut to his/her skin during the surgery.
- We do not recommend planned caesarean sections before 39 weeks as babies have a higher risk of being admitted to the special care baby unit for breathing support.
- Caesarean section will have implications for any future pregnancies that you may have. This is explained in more detail later in this leaflet.
Preparation for a planned caesarean birth
After you have received balanced counselling about your birth choices, if you wish to proceed with an elective caesarean section, you will be asked to sign an electronic consent form.
You will then have an appointment arranged in our Pre-op clinic and your caesarean will be listed at the recommended gestation. The pre-op appointment takes place approximately 1 week before your scheduled delivery time. We will give you some information on how to look after yourself before and after the caesarean, along with obtaining a sample of blood to check for anaemia and a skin swab to check for MRSA. More information about MRSA can be found on our website under Infection Prevention and Control > MRSA.
At the pre-op clinic, you will be given a medication called Omeprazole. This helps to reduce the amount of acid in your stomach and the volume of fluid in the stomach.
Planned caesarean section:
Morning surgery planned: Take 2 x 20mg capsules (40mg) at 10pm the night before and take 2 x 20mg capsules (40mg) at 6am on the morning of the planned caesarean section.
Afternoon surgery planned: Take 2 x 20mg capsules (40mg) at 6am and take 2 x 20mg capsules (40mg) at midday on the morning of the planned caesarean section.
The anaesthetic team will discuss the safest option of anaesthesia for you. It is most often recommended that you stay awake for your surgery by having a spinal anaesthetic. This means that you can have a support person to remain with you during your time in theatre.
A spinal anaesthetic is stronger than an epidural and makes you numb from the top of your tummy to your feet. You may be aware of some movement, but you should not feel any pain. The anaesthetist will remain with you at all times during your delivery and you can discuss any concerns that you have. After the spinal anaesthetic has been placed, your midwife will place a small tube into your bladder (bladder catheter). This will remain in place until you are up and about again after your caesarean.
You will have a drip placed in the back of your hand and given fluids to help keep you hydrated until you are eating and drinking again. Once you are eating and drinking the drip can be stopped. The cannula can be removed once the midwife caring for you is happy that you are safe and well.
Your birthing partner will be allowed to sit with you at the head end of the operating table. They will be given a theatre gown to wear over their own cloths to minimise the risk of infection. A screen will be put up so that neither of you can see the operation. This screen can be temporarily lowered at the point of birth if you wish. Please let us know if you would like us to do this.
If all is well, we usually offer delayed cord clamping and skin to skin as soon as possible following the birth.
The usual amount of time in theatre is approximately 60 – 90 minutes.
More information about your anaesthetic can be found on our website under Anaesthetics > Patient journey > Information leaflets.
Care following your caesarean section
Afterwards, you will be taken to a recovery room for at least 30 minutes. You can continue skin to skin during this time if all is well.
Once on the ward, your partner is permitted to stay 24 hours a day and will be asked to sign a visitors contract. There are additional visiting hours available for other friends / family who may wish to visit you.
Please bear in mind, that whilst we understand that this an exciting time, you have just undergone a major operation and having a quieter day following the birth of your baby is often more helpful for your recovery.
You will be offered different methods of pain relief on the postnatal ward and for your return home. Regular pain relief is recommended to aid your recovery and to keep you as comfortable as possible. There is often more pain associated with recovery from caesarean section than vaginal birth. Approximately 90% of people who have had a caesarean are pain free by 6 weeks. 10% of people will continue to experience pain for the next few weeks or months. You can watch a video or access a leaflet on the Liverpool Women’s NHS Trust Internet page under Maternity/Maternity Patient Information Leaflets/Maternity Leaflets about your analgesia options.
We recommend staying in hospital for 24 – 48 hours after your caesarean section.
The midwives and support staff will help you to mobilise soon after your birth to prevent blood clots. Do not get out of bed for the first time without a member of staff to support you. Once you have been out of bed and feel confident walking, your bladder catheter can be removed.
The midwives will check on you regularly to ensure that you and the baby remain safe well.
The midwife caring for you on the ward will help and advise you on how to care for your wound/scar. The stiches are usually dissolvable, but we will provide specific advice following your birth, once on the postnatal ward.
Birth by caesarean section typically requires a longer recovery period than vaginal delivery. We recommend a recovery period of 4-6 weeks. During this time, we recommend that you don’t lift or push heavy objects.
We recommend that you do not drive during this time. It is advisable to check your car insurance policy with your individual insurer.
Implications for future births
There is an increased risk that the placenta can be positioned lower in the womb (placenta praevia) in future pregnancies. The placenta can be very adhered to the lining of the womb, which makes delivering the placenta more difficult. This increases the risk of heavy bleeding next time.
There is a small chance that the scar on the womb can re-open during labour with subsequent pregnancies. The risk is approximately 0.5% or 1 in 200 times. This would only be a concern if trying for vaginal birth next time.
There is a slight increased risk of future stillbirth: 1- 4 per 1000 births.
You will be able to ask any questions you may have at any time throughout your stay.
For further information please ask your midwife. Other resources:
- RCOG Considering a caesarean birth.
- RCOG Birth options after a previous caesarean.
This information is not intended to replace discussion with either medical or midwifery staff. If you have any questions regarding the contents of this leaflet please discuss this with your midwife or obstetrician.
Induction of Labour
Bitesize Leaflets
How your labour can be induced
Pain relief during induction of labour
PROM (Pre-labour Rupture Of Membranes)
Where your Labour can be induced
Why Induction of Labour - prolonged pregnancy
The links below are relating to national leaflets which are deemed appropriate for services that we at LWH provide.
Please note: The formatting of these leaflets are mandated nationally and LWH does not have the authority to amend these.
Screening Leaflets
Antenatal Screening Websites
Food Information Websites
Group B Strep Websites
Sickness and Vomiting Websites
Caesarean Section Websites
