The leaflet is detailed below, or you can download the 'Neonatal Unit - Information for Parents' leaflet in PDF.
The staff on the Neonatal Unit at Liverpool Women’s NHS Foundation Trust would like to extend a warm welcome to you and your baby.
We recognize that this is a difficult time for you and we know that however small or sick your baby is, you, the parent(s) are the most important people in your baby’s life.
We will do everything we can to support, inform and guide you throughout your time here.
Location of Unit
The Neonatal Unit is situated on the first floor of the hospital opposite to Delivery Suite and next to the Maternity Base.
The Neonatal Unit provides expert care for new-born babies who are unwell. It offers specialised care for:
- Babies born prematurely
- Babies with health problems diagnosed before birth (antenatally) or after birth (postnatally)
- Full-term babies who have become unexpectedly unwell
Access to the Neonatal Unit and Security
To gain access to the unit you must press the corresponding button for the room where your baby is being cared for, on the intercom system outside the main door to the Neonatal Unit. Staff will check your details and who you have come to see, before letting you in. If you are unsure, press ‘Reception/ The Hub Reception” and the Ward Clerk will check your details and allow you access. Please be aware that they are not on duty overnight so if there is no response, please press for one of the other rooms and someone will help you.
For the safety and security of your baby, please do not let any other person come in the door behind you or open the door for another person.
Infection Control
We aim to provide a safe and clean environment. The following applies to parents and visitors
- Remove all outdoor coats and handbags / bags and leave in the lockers provided before entering the nursery.
- Please do not leave any valuables unattended in these areas, as the Trust cannot be held responsible for any loss. Lockers are provided for parents at the main entrance, the digital code for these will be given to you on arrival and you can keep this locker for the extent of your stay.
- Remove all watches, bracelets and rings (except plain wedding rings) and roll up your
- Then please ensure you wash and gel your hands thoroughly at the hand washing troughs on the main corridor before you proceed into the unit.
- Before entering the any of the clinical rooms apply the alcohol hand gel again which is located by the
- After entering the room, please wash and dry your hands and reapply the alcohol
- Remember to always gel your hands before and after touching your
- When leaving the room reapply the alcohol gel again using the gel located outside each door.
- Each time you return to the room you must repeat this
Staff and parents are regularly monitored for effective hand hygiene. Please contact a member of staff if you have any concerns.
The Neonatal Unit is divided into three areas; a designated Neonatal Consultant oversees the care and treatment of babies in each of these areas:
- Neonatal Intensive / High Dependency
- Low Dependency (LD)
- Transitional Care (TC)
Neonatal Intensive/ High Dependency
This critical care area provides support for babies who have breathing problems, are recovering from surgery or require other specialist treatments.
There is a range of specialist equipment to help care for your baby in these rooms. For more information about the equipment used on a neonatal unit please visit the Bliss website or see the Bliss Parent Information booklet. If you have not received this in your admission pack, please speak to a member of your neonatal care team.
Once your baby is getting better and needs a little less nursing support, they will be transferred to Low Dependency (LDU).
We also have rooms for consultations and meetings with parents if not able to meet at the cotside.
Ward Rounds in the Intensive / High Dependency Rooms
Each day there is a ward round led by a Consultant. You are welcome to stay in the room throughout but we ask that you wear headphones until your baby’s condition is being discussed to avoid breaches of confidentiality.
Ward Rounds in the Low Dependency Rooms
In the Low Dependency rooms there is a ward round Monday, Wednesday and Friday. You are welcome to stay in the room but we ask that you wear headphones until your baby’s condition is being discussed to avoid breaches of confidentiality. A weekly discharge planning meeting is held on Wednesdays to discuss plans for discharge home.
The nurse looking after your baby will let you know what time these rounds take place.
Nursing Hand-Over Times
Nurses’ hand-over times are 07:15 hours and 19:15 hours. The handover takes approximately 15-30 minutes. You are welcome to stay in the room but again we ask that you wear headphones to avoid breaches of confidentiality.
Transitional Care
Transitional care is an area for mothers who are well following delivery, to care for their low birth weight baby and those babies born after 34 weeks who do not need specialised care. This is done with the additional support and encouragement from the Transitional Care Team who provide care that exceeds normal routine care. It is located on the Maternity Ward.
The Transitional Care Team is led by a Team Leader, Registered Neonatal Nurses/ Midwives, and Clinical Support Workers. They support and educate parents in caring for their baby in preparation for home. In addition, the team also supports midwifery staff in problem solving in the maternity ward to prevent unnecessary separation of mother and baby.
The Neonatal Medical team will provide medical care for your baby whilst on Transitional care.
Neonatal Community Outreach Team (NCOT)
Alongside the Transitional Care Team, the Outreach Team will work closely with you to make sure that you feel confident to care for your baby when you go home.
This is a team of Neonatal Nurses who will provide support and advice for premature babies and babies whose weight is less than 2.3 kg at discharge. The team will monitor your baby’s progress in the community before discharging you to the Health Visitor. The team will also carry out any necessary blood tests your baby may need, and help you access specialist teams and community services if required.
Follow-Up Care
Some babies who are admitted to the Neonatal Unit for a short time do not need any follow-up care after they are discharged. Others however will have a follow-up appointment with one of the Consultants at about four to six weeks after leaving the unit. This will take place at Liverpool Women’s Hospital. Babies who are born very premature, or are very unwell, will have follow-up appointments at the Liverpool Women’s Hospital and the Alder Hey Children’s Hospital. The appointments will continue for at least two years so that staff can closely monitor the development of your baby.
Staff
The Neonatal Unit is staffed by a highly skilled team who are dedicated to giving your baby the best possible care.
Doctors
There is a team of Consultant Neonatologists. These doctors are responsible for the care of newborn babies who need extra support shortly after birth. They also supervise a team of paediatric junior doctors, and provide 24-hour emergency and specialist care. They will carry out most of your baby’s routine medical care. If your baby needs an opinion from another Specialist, the doctors from that team may see your baby in the Neonatal Unit, or in their clinic once your baby has gone home.
If you have any questions about your baby’s progress, you can ask the doctors on a daily basis. You can also request a meeting with a Neonatal Consultant who will be happy to discuss your baby’s care with you.
Advanced Neonatal Nurse Practitioners
A team of Advanced Neonatal Nurse Practitioners (ANNPs) work alongside the medical staff. They are very experienced Neonatal Nurses who have undertaken additional specialist training to enable them to examine, diagnose, request investigations, and perform any of the procedures performed by medical staff.
Nurses
The Neonatal Unit has a Head of Neonatal Nursing and a Matron who are in charge of this large number of Nursing staff and Clinical Support Workers in the unit who specialise in looking after sick or premature babies. The staff will update you each time you visit on your baby’s progress. There is also a Shift Leader available 24 hours a day on the unit who has overall responsibility for the care delivered during that period.
Radiographers
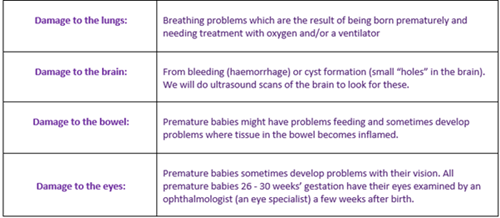
Radiographers are health professionals who take X-rays of your baby. This is to identify and monitor diseases, bone and soft tissue abnormalities and is also necessary to check the position of your baby’s Intravenous lines and tubes.
Ophthalmologists
Ophthalmologists are doctors who specialise in eye care. They visit the unit every Tuesday. All babies born under 31 week’s gestation and or 1.501kg are referred to the Ophthalmologist as part of a national screening programme. An appointment for your baby to be seen by the Opthalmologist will be given to you.
Physiotherapist
A Neonatal Physiotherapist‘s role is to support the development of babies who may be at risk of having movement or developmental difficulties. They will assess your baby and give advice to you and the nursing staff on developmentally supportive care, including, handling and positioning that is specific for your baby. For some babies they will also be involved in neuro-developmental follow up post discharge to ensure the baby is developing their gross motor skills appropriate to their age.
Pharmacists
Pharmacists visit the ward on weekdays (Mondays to Fridays) to review your baby’s medication. You can ask them for more information about your baby’s medicine should you wish.
Liaison Health Visitor
The Liaison Health Visitor is responsible for informing your Health Visitor about your baby’s admission, progress and discharge plans. All families with a new baby will have contact with a Health Visitor close to their home that will be there to provide support and advice on child and family health matters.
Counselling/Support for Parents
We understand that having a sick or premature baby can be extremely stressful for parents and so we can offer you support through our family support counsellor or psychology service, please ask your baby’s nurse for more information.
Spiritual Team
Our spiritual team supports people of all faiths and beliefs, as well as those who do not have a particular religious belief. A member of the hospital chaplaincy team also visits the unit several times a week, if you would like to have a Baptism or naming ceremony arranged please ask the staff who can contact them on your behalf at any time.
Research
There is an experienced research team who are committed to advancing medical care through improved knowledge and understanding. A member of the research team may come to discuss with you about becoming involved in a research study.
Students
Medical students spend some time on the neonatal unit as part of their basic training and qualified doctors have placements here as part of their ongoing professional development. Student Nurses and Midwives also have placements here as part of their training. They are allocated to a Nurse and will care for your baby under the nurse’s supervision and with their assistance.
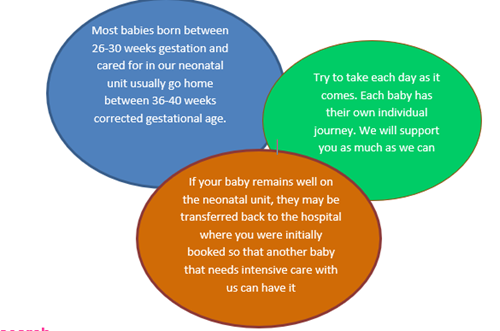
Transfer of Care
The Neonatal Unit at Liverpool Women’s NHS Foundation Trust specialises in looking after babies who require intensive care. When your baby no longer needs intensive care, we will arrange for your baby to be transferred back to your local hospital. This will happen even if you have planned to have your baby at Liverpool Women’s Hospital but have a nearer hospital, or if you have been referred here for your baby’s specialist care before birth.
Transferring your baby back to your local hospital is beneficial for many reasons: It makes it easier for you and your family to visit your baby, it allows the doctors at your local hospital to get to know you and your baby and it allows for your baby’s follow-up clinic appointments to be organised.
We understand that the idea of your baby being transferred to another hospital can be stressful. Please be assured that we only arrange the transfer when we are sure that it is the right time for your baby.
Transferring babies back to their local hospital helps us to provide specialised intensive care to those babies who need it most, like your baby did when they were first born. It is possible for you to visit your local unit before the transfer. If you would like to do this, please speak to the staff caring for your baby.
Caring For Your Baby
Staff will involve you in the care of your baby as soon as possible. You may feel a little apprehensive about touching your baby at first, but staff will help you to gain your confidence.
It is very important that you have contact with your baby. At first it may only be a touch, but as soon as baby’s condition allows you will be able to have a cuddle and perhaps have skin to skin contact which is sometimes called Kangaroo care. This is especially beneficial for Mum and/or Dad as well as baby.
The staff will guide you on what is appropriate for your baby at different stages of their development.
You may feel a little apprehensive about touching your baby at first, but staff will help you to gain your confidence.
Breastfeeding
The staff actively support a mother’s choice to breastfeed her baby whenever possible. Breast milk is the best option for your baby, particularly when they are born prematurely or are unwell.
Breast milk is much easier for babies to digest than formula milk and helps protect your baby from infections. Very small babies only need very small amounts of milk, so any milk you produce can be given to your baby.
There is a room in the unit where mothers can express their milk in private. There are also screens/ curtains in the rooms so that you can express beside your baby. Bonding squares are provided to all mothers on admission to the unit. Each mother is given two squares, one is kept with their baby and one is kept on the mother’s body. They help the mother and baby to bond by smell and help mothers who are expressing in the stimulation of oxytocin, the “let down reflex”.
Skin to skin contact will help mothers who are expressing increase her oxytocin levels for breast milk production and is great step towards breastfeeding. Skin to skin contact enhances feelings of affection between mother and baby and promotes bonding.
If your baby is not having large amounts of milk to start with, it is perfectly safe for it to be frozen and stored until the time when the baby needs it. There are freezers available to store the milk. You will need to clearly label each container of expressed milk with your baby’s name, date of birth, hospital number and the date and time it was expressed.
The Nurse looking after your baby will give you advice and support on expressing milk and breastfeeding. Support is also available through the Neonatal Breast Feeding Team.
The unit offers high quality electric breast pumps available on a loan basis, free of charge but must be returned before your baby is discharged. This service enables mothers to express their milk when they have gone home and bring it to the neonatal unit for their baby - a very practical way in which mothers can contribute to their baby’s development and growth in the crucially important early days and weeks of life.
Two parents room are available on the Neonatal Unit where mothers can ‘room in’ with their baby to establish breastfeeding when getting ready for home.
Donor Breast Milk Bank
We also understand that this can be a stressful environment and establishing a good milk supply can be difficult. This is where the donor breast milk bank proves invaluable. Donor mothers (who have more milk than their babies need) can give milk to the milk bank, where it is pasteurized, stored and supplied to neonatal units.
The medical team will discuss with you whether your baby would benefit from donor breast milk and will always ask for your consent (permission) before giving donor milk to your baby.
Visiting
We operate an open visiting policy for parents and baby’s own brothers and sisters. No other children are allowed.
There is a play area within the sitting room with toys for brothers and sisters of babies on the unit. Because of the small space and the potential for hot drinks being accessible, children must be supervised at all times.
Visiting hours are displayed in the unit and you can ask your baby’s nurse for this information. A maximum of two visitors per day may come to the unit and see your baby (A maximum of 4 people in each bedspace) in order to minimise the risk of infection to your baby. Siblings are not included in this total of visitors per day. If large number of siblings are visiting together, please speak to shift leader and we will try to accommodate the best we can. No visitors allowed without at least one parent present. Please respect these precautions. If this causes extreme difficulties, please speak to the Shift Leader.
Visitors should not visit if they are unwell e.g. have a cold, flu, stomach upset. If you are unsure if your visitor should visit, please phone and check with the nurse looking after your baby. They must not visit the unit wearing a uniform from another healthcare setting as this increases the infection risk to the baby.
Information about the Unit
Toilets
Toilets including a disabled toilet are situated the main corridor of the unit. Baby changing facilities can be found in one of these inside the entrance to the unit
Unit Cleaning
Each day the domestic staff needs to have access to the clinical area to maintain the high standards of cleanliness required for this Neonatal Intensive Care Unit.
Parking Facilities
Contained in the admission pack is a leaflet concerning car parking. Authorisation can be given to parents to park in designated areas without charge. Please make sure you get this form signed by the Shift Leader as this will instruct staff on the main hospital reception to issue you with a card after each visit to allow you to leave the car park without charge.
Phoning
Parents can telephone any time day or night and we will not give out information to anyone else.
The hospital phone number is: 0151 708 9988 if you know the room number where your baby is being cared for, chose Option 5 and the extension of the that room (listed below) if not, then choose Option 0, then ask the switch board operator to put your call through to the neonatal reception.
Room 1 – 1201 Room 2 – 4652
Room 3 – 4505 Room 4 – 4506
Room 5 – 4507 Room 8 – 4500
Room 7 – 1732 Room 9 --1705
Transitional Care - 1042
Between 08:00 – 16:00 hours only you can ring on a direct line number to the reception desk on 0151 702 4193 but this is not staffed after this time. Please ensure we have your phone number in case we need to contact you. (NB: We may have difficulty contacting you on a mobile phone, so an alternative land line number should be given where possible).
Other Things to Know
The Nurse allocated to help you care for your baby is responsible for all the care delivered on that shift so we ask that parents do not cancel alarms, adjust oxygen levels, Intravenous or oral feeding tubes. Unauthorised changes can cause harm to your baby sometimes with very serious consequences.
Individuals who put baby’s health at risk by unauthorised adjustment of treatment will be excluded from the unit.
Red Trolleys
Please do not disturb the staff, except in an emergency, when you see them working at a red trolley as they are calculating, preparing or administrating complex medication therapies for babies and need to concentrate so they do not make a mistake.
Nappies and Cotton Wool
Parents must provide their own disposable nappies and cotton wool for their baby during their stay on the Neonatal Unit. Most large supermarkets and chemists stock premature nappies and you can also buy them on the internet. The very preterm nappies will be provided as these are not easily available to buy.
Quiet Time
Although the nurseries can be very busy we aim to keep the Neonatal Unit environment as quiet as possible and we would ask that you and your visitors help us achieve this.
Drinks in the Nurseries
Hot drinks are not permitted in the nurseries. Water in a sealable bottle/ container is allowed.
Baby Clothing
We have a stock of baby clothes, which are washed on the premises.
You can bring your own clothes for your baby, but they must be labelled with your baby’s name and the family must take them home to wash.
It is recommended that the clothes are washed at no lower temperature than 60º centigrade and that they are tumble-dried.
Toys
Toys are not allowed in incubators/ cots whilst the baby is in the Intensive Care/ High Dependency area however a comfort cloth can be used. In the Low Dependency areas, two small washable toys can be left in the incubator/ cot if the baby does not have any Intravenous lines in place. These should be taken home and washed weekly.
Comfort Cloths
If you hold a cloth close to your body, you can transfer your unique smell to your baby who will be comforted when the cloth is placed next to him/her. You also will be comforted if you take a cloth home with your baby’s smell on it and if you are expressing it will help your milk to flow
These cloths must also be washed frequently at 60º Centigrade.
Strong smells including strong perfumes will be too stimulating for your baby, so please try to avoid them.
Use of Dummies
The staff will ask for permission to use a dummy while the baby is not receiving any milk feeds as this helps develop the sucking process and will help the baby reach full milk feeds more quickly.
Dummies can also be used as a method of pain relief during short procedures such as taking blood from a heel prick.
Dummies must be washed with hot soapy water, rinsed, dried and stored in a small container between uses. Dummies provided in hospital MUST NOT be taken home and used after discharge.
It is helpful if parents bring in sterilised bottles and teats prior to discharge home so the baby can get used to them and the staff can advise if any concerns are raised with their use.
Baby Diary
This is an online diary that contains photos and short messages. Should parents wish to use this facility, they will be able to access the diary using a user name and password of their choice, the nurse caring for your baby will be able to organise this for you. Parents will then be able to review photographs and diary entries about their baby wherever they wish.
This will be subject to availability of staff time to make entries.
Tests
There are a variety of routine tests that premature babies will have on the unit; further information is available, just ask a member of staff.
Blood Spot Screening
On admission to the unit your baby will have a sample of blood taken for blood spot screening. A further sample will be taken along with any routine blood due between day 5 and day 8 of life. This is a national test to check for blood disorders such as phenylketonuria (PKU), hypothyroidism, Sickle cell anaemia and cystic fibrosis as early recognition and treatment is essential for babies with these disorders.
If your baby is born less than 32 weeks gestation they will need a repeat sample taken on day 28 of life or at discharge. If you do not wish you baby to have these tests please tell the nurse or doctor looking after your baby.
You should have received a leaflet about the blood spot test in your antenatal information pack. If you have any further questions ask the nurse or doctor to explain it to you.
Screening
All infants will have their hearing checked prior to discharge as part of a national screening programme.
You should have received a leaflet about the blood spot test in your antenatal information pack “Planning For Leaving Hospital”. The nursing staff will discuss this with you at the appropriate time when the test is due.
As your baby becomes more stable and is able to control their temperature, they will move from an incubator to a cot. The machines monitoring heart rate and oxygen levels will no longer be needed and will be replaced by monitors which check your baby’s breathing. These will be removed before the baby is discharged.
As your baby matures, or condition improves, we will want to try and encourage them to take feeds by mouth. The change from tube feeds (liquid nutrients passed down a tube from the nose into the stomach) or intravenous feeds (nutrients passed into a vein) might start slowly by introducing one feed per shift, by your chosen method (breast or bottle). Then the frequency and the amount of milk are increased.
As your baby gradually progresses from one to three-hourly feeds, your presence becomes even more important. Your baby needs to learn the technique of feeding, by breast or bottle, and so do you. By being present at feed times you will get used to your baby’s feeding style and your confidence will grow.
Visiting during the day also helps to develop your baby’s sense of a day/ night cycle. When you are at the unit during the day, we encourage you to care for your baby whenever possible.
Hearing you and seeing you is good stimulation, and aids your baby’s development.
There are fewer chances to interact with your baby at night-time. Babies are only handled for feeding, changing, or if they are unusually unsettled.
Information and Support for Parents
There are many organisations which offer information and support for parents. You should have received the Parent Information Guide produced by Bliss – if you have not, please ask us for a copy. It includes contact details and website addresses of organisations and support groups, which can help you while your baby is in the unit, and when your baby goes home.
The Bliss helpline offers support by telephone, text or email. Champions and Buddies are often parents that have also had a baby on a neonatal unit and may have had similar experiences to you. Please see the posters around the unit for more information. You will find that all the staff are very supportive but if you would like to talk to someone else, the following people may be able to help:
Peer support from other parents can be accessed by joining the closed Facebook site “Neomates- Liverpool”
There is a Shift Leader available 24 hours a day on the unit. The Matron is available Monday - Friday
If you wish to speak to a Consultant or Doctor please tell the nurse caring for your baby. An interpreter service is also available and the staff caring for your baby can organise this.
There is also the Patient Advice and Liaison (PALS) Manager, extension 4353.
Accommodation
Within the unit are two parents’ bedrooms, these are for short-term use only and are in great demand. Siblings cannot stay in these facilities. If you are staying, we ask that you vacate the room for a short time at 11.00 hours each day, to have your bed put up and the room cleaned. For safety reasons please do not try to put the bed into the upright position yourself.
The rooms are used to assist parents in preparation for home. If you wish to stay, ask your nurse who will book the room for you if it is available.
In the event of a baby being very sick you may have to move at short notice so that other parents can be close to their baby.
There is also parent accommodation on the second floor – directly above the neonatal unit and this is offered when your baby is requiring intensive care subject to availability. Cereal / toast / tea and coffee are provided along with a small range of tinned / dried items for you to use.
Siblings cannot stay in these facilities.
If your stay is thought to be more long term there is also some offsite accommodation, these have kitchen facilities and a sitting room and can be arranged via the Shift Leader but please note that there is only one flat with facilities for siblings to stay. This is means that the provision is reviewed every 2 weeks so that other families can use this accommodation and you may be asked to move to another flat without facilities for siblings.
Parents must cater for themselves and keep the accommodation clean and tidy as they are only cleaned by the unit staff on departure in preparation for other parents to use.
Parents who fail to keep the accommodation to an acceptable standard or whose behaviour is inappropriate whilst staying here will be asked to leave immediately. No alternative accommodation will be arranged by the Neonatal Unit.
Visitors are not permitted on these premises. Smoking is only permitted within designated smoking shelters on the hospital site and is not permitted at all in the offsite accommodation.
Food for Parents
If you are staying in one of the two onsite parent’s bedrooms, breakfast items and a small range of tinned/ dried foods are provided. Alternatively you can bring your own food and use the parents’ kitchen which has a toaster, microwave and refrigerator. Please clean the area after use. If you are visiting during the day you can bring your lunch and store it in the fridge. Please put the date on as all food not labelled and /or more than 24 hours old will be discarded for health and safety reasons.
If you arrive out of hours and are resident in the parent rooms and have missed a meal, snacks can be obtained for you, please ask the Shift Leader if required.
Food is also available in the restaurant, cafe and from the shop in the foyer – please check the opening times displayed outside these venues.
Family Information
Information can be found on the trust website and a QR code can be found on the notice board. If you cannot find anything you feel you need, please ask the nurse caring for your baby.
Picture Board
Parents love to look at the photos in the gallery and see how premature babies have grown. If you wish your baby to be in the gallery don’t forget to send your story/photo into the Matron on the neonatal unit.
Registering Your Baby’s Birth
You can register your baby at the Liverpool Register Office. You can book an appointment online or contact Tel: 0151 233 3004.
A baby’s birth must be registered by law within 42 days (6 weeks).
Registering your baby with your local GP
Before discharge ring your GP for a registration form and to register your baby. This is important if you baby requires any medication on discharge.
Fire Alarm and Generator Testing
The fire alarm is tested once a week. If the alarm goes off please stay by your baby however if you are in the sitting room or the bedrooms on the unit, please return to the room where your baby is being cared for and await further instructions from nurse in charge of the room.
Generator testing also takes place monthly; this sometimes causes the baby’s alarms to go off but there is no danger to baby and the staff will be aware of this happening.
Travel
- Mersey Travel Travelline telephone: 0871 200 2233
- National Rail enquiries: 0845 748 4950
- Taxis are available outside main hospital entrance
- More Travel information can be found at the main hospital
- Hospital Telephone number: 0151 708 9988
Address: Neonatal Intensive Care Unit, Liverpool Women’s NHS Foundation Trust, Crown Street, Liverpool L8 7SS.
Visitor Waiting Areas
Visitors who do not have access to the unit can wait on the main hospital corridor and should not try to enter the unit for safety and security reasons.
To the left as you enter the unit the is a small bench for visitors to wait if they are asked to leave the clinical area for any reason, they should not wait in the main corridor as this is constantly in use by staff and needs to be clear in case of an emergency.
If visitors require access to baby feeding facilities these are available in the main foyer – please ask at the Main Reception on the ground floor for the key.
Developmental Care for Your Baby
Developmental care promotes each baby’s comfort and sleep in a way that reduces the stresses of the Neonatal Unit environment. This includes the use of positioning and handling techniques, reducing the discomfort of the Neonatal Unit environment (noise and light levels) so ensuring that your baby is as comfortable as possible.
Family Integrated Care (FiCare)
This is a model of care planning and delivery encouraging parental involvement as partners in their baby’s care. As part of this, we have 3 pledges that we will ensure we maintain. These are
- You will be first to give your baby their first oral feed
- You will be first to dress your baby
- You will be first to bath your baby.
Baby Steps Cards have been introduced which will enable parents to document skills that they have gained. This will allow for good communication and consistency across nursing staff and units within the neonatal network.









 Feeding
Feeding