The leaflet is detailed below, or you can download the 'Infection Prevention & Control Service General Patient' leaflet in PDF.
Picking up an infection in hospital is a concern for many patients. Although most patients do not get an infection Liverpool Women's Hospital NHS Foundation Trust (LWH) is committed to reducing infection rates to an absolute minimum.
This leaflet aims to provide information about infection at LWH, what you should expect from the Infection Prevention & Control Service and what you can do to help protect yourself and your visitors from infection.
Infections are mainly caused by viruses and bacteria commonly known as ‘bugs’ or germs.
Most germs are in the environment and are harmless. Sometimes when we are in hospital there is an increased risk of the germs entering our bodies e.g., intravenous lines (drips), catheters, surgical wounds. The germs can be passed from one person to another by physical contact.
Health care workers, visitors and patients reduce this risk by regularly cleaning their hands.
Infection Prevention Service
The Director of Infection Prevention & Control and the Infection Prevention Team are health professionals trained in infection control and prevention. They advise the ward staff on all aspects of patient care when infection may be a risk.
The Trust has an Infection Prevention & Control policy which all staff must follow when providing care to patients.
The Infection Control Team produce an Annual Report for the Trust which demonstrates the numbers of hospital infections detected and what actions are being taken to prevent infections.
This report can be viewed on the Trust website
https://www.liverpoolwomens.nhs.uk/
The Trust has very low levels of hospital acquired infections. Information on MRSA bacteraemia (blood stream infection) is monitored by the department of Health. This Trust is amongst the lowest in the Northwest and nationally for this serious infection. All patients admitted to the gynaecological ward are screened/swabbed for MRSA as are all pregnant women who are booked to have a caesarean section.
Diarrhoea acquired in hospital can be caused by a bug called Clostridium Difficile Toxin (also known as C. diff or CDT). LWH once again has very low levels of this infection.
Wound infections are more common than either MRSA or C diff. It is difficult to collect accurate information as patients may be discharged with a wound which is healing well but becomes infected in the community after discharge home. (Current information on all types of infection and prevention can be found on the notice board in the Trust’s main reception).
What You Can Do to Help
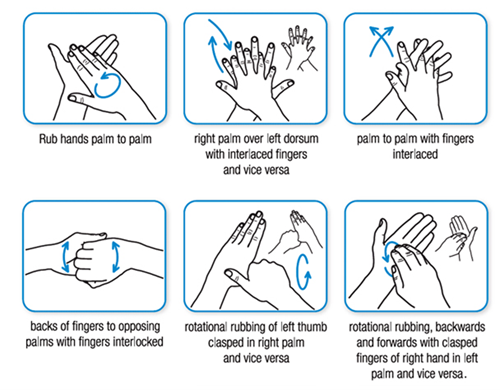
All health care staff are trained in hand hygiene and are expected to carry out this technique before each patient contact or procedure. If they forget to do this, they will be happy for you to remind them. If you wish, the staff will be happy to demonstrate the correct technique for hand washing. It is important hands are cleansed when:
- Entering and leaving the ward area.
- Before eating.
- After toileting or using sanitary products.
- Whenever you can see your hands are dirty.
- After visiting a patient who is known to have an infection.
- If you have wounds, dressings or catheters try not to touch them more than necessary.
- If you have a cough, cough away from your wound.
Hands can be cleansed using soap and water when visibly dirty or after using the toilet. At all other times hands can be cleaned with hand gel. The gel is provided at your bedside for your use and the use of the staff and visitors.
Please tell the nursing or medical staff if you have had any of the following in the week before admission:
- Diarrhoea or vomiting
- Flu-like illness
- An unexplained rash (or contact with someone with a rash)
If you have any questions about the risk of infection associated with your surgery/procedure, please ask the nurse/midwife or doctor caring for you they will be pleased to discuss any concerns you have.
If you have concerns regarding infection or infection prevention, please speak to the nurse looking after you. You can also discuss your concerns with a Matron or a member of the Infection Prevention & Control Team on 0151 702 4014.
Trust Information Leaflets are Available on the Following Topics:
Hand Hygiene
Hand Hygiene - Neonatal, Guidance for Parents and Visitors
Helping care for your Wound.
Carbapenemase-producing Enterobacterales Screening
Carbapenemase-producing Enterobacterales Positive Result
Clostridium difficile
MRSA
Health Protection Agency Leaflets:
Noro virus