The leaflet is detailed below, or you can download the 'You and your Anaesthetic' leaflet in PDF.
Information to help patients prepare for an anaesthetic
This leaflet gives information to help you prepare for your anaesthetic. It has been written by patients, patient representatives and anaesthetists, working together.
You can find more information leaflets on the website www.rcoa.ac.uk/patientinfo. The leaflets may also be available from the anaesthetic department or pre- assessment clinic in your hospital.
The website includes the following:
- Anaesthesia explained (a more detailed booklet)
- Your anaesthetic for major surgery
- Your spinal anaesthetic
- Epidural pain relief after surgery
Risks associated with your anaesthetic
Below are specific risks associated with having an anaesthetic or an anaesthetic procedure. It supplements information available on the website: www.rcoa.ac.uk/patientsinfo
Side effects and complications
Regional Anaesthetic (RA)
General Anaesthetic (GA)
More information on the side effects and complications than is listed here
can be found on the website (www.rcoa.ac.uk/patientinfo
RA = This may occur with a regional anaesthetic
GA = This may occur with a general anaesthetic
Very common and common side effects
RA GA = Feeling sick and vomiting after surgery
GA = Sore throat
RA GA = Dizziness, blurred vision
RA GA = Headache
RA GA = Bladder problems
GA = Damage to the lips or tongue (usually minor)
RA GA = Itching
RA GA = Aches, pains and backache. Pain during injection of drugs. Bruising and soreness where a needle was inserted in order to give fluids or medication (usually after the tube/cannula is removed).
GA = Confusion or memory loss
Uncommon side effects and complications
GA = Chest infection
GA = Muscle pains
RA GA = Slow breathing (depressed respiration)
GA = Damage to teeth
RA GA = An existing medical condition getting worse
GA = Awareness (becoming conscious during your operation) - This is more likely to occur during a sedation technique where the aim is to allow the procedure to be performed with the best recovery profile.
Rare or very rare complications
GA = Damage to the eyes. Heart attack or stroke. Serious allergy to drugs. Nerve damage
RA GA = Death
RA GA = Equipment failure
Deaths caused by anaesthesia are very rare. There are probably about five deaths for every million anaesthetics in the UK.
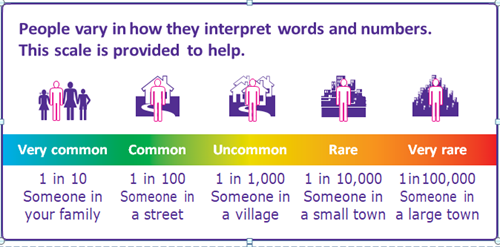
Understanding risk
In modern anaesthesia, serious problems are uncommon.
Risk cannot be removed completely, but modern equipment, training and drugs have made it a much safer procedure in recent years.
To understand a risk, you must know:
- how likely it is to happen
- how serious it could be
- how it can be treated.
The risk to you as an individual will depend on:
- whether you have any other illness
- personal factors, such as smoking or being overweight
- surgery that is complicated, long or done in an emergency.
More information about risks associated with having an anaesthetic can be found on www.rcoa.ac.uk/patientinfo
What is anaesthesia?
Anaesthesia stops you feeling pain and other sensations.
It can be given in various ways and does not always make you unconscious.
Local anaesthesia involves injections that numb a small part of your body. You stay conscious but free from pain.
Regional anaesthesia involves injections that numb a larger or deeper part of the body. You stay conscious but free from pain.
General anaesthesia gives a state of controlled unconsciousness. It is essential for some operations. You are unconscious and feel nothing.
Anaesthetists
Anaesthetists are doctors with specialist training who:
- discuss the type or types of anaesthetic that are suitable for your operation. If there are choices available, your anaesthetist will help you choose what is best for you
- discuss the risks of anaesthesia with you
- agree a plan with you for your anaesthetic and pain control
- are responsible for giving your anaesthetic and for your wellbeing and safety throughout your surgery
- manage any blood transfusions you may need
- plan your care, if needed, in the intensive care unit
- make your experience as calm and pain free as possible.
The pre-assessment clinic
If you are having a planned operation (rather than emergency) you will usually be invited to a pre-assessment clinic a few weeks or days before your surgery.
Staff at the clinic will assess your general health. You will be asked questions and a nurse or doctor may listen to your heart and lungs. Tests will be organised if necessary. This will often include blood tests and an ECG (heart tracing).
You are likely to be checked for certain important infections – usually by using a swab on your skin, or in your nose.
The staff will want to make an accurate list of the medicines you take. Please bring a list or the medicines themselves in their boxes.
If you are allergic to anything, this will be written down.
If necessary, arrangements may be made for you to see an anaesthetist.
If you may need a blood transfusion during or after your operation, a blood test will be needed to prepare for this. You can ask for information about the risks and benefits of blood transfusion. Blood transfusions are generally avoided unless necessary.
If you know you have high blood pressure, it is a good idea to bring a list of any recent blood pressure readings. This is because blood pressure can rise in a hospital clinic, and this may not be a true picture of your usual blood pressure.
More information
This is a very useful opportunity for you to ask any questions that you have about the anaesthetic and about coming into hospital generally. If the staff do not have all the answers you need, they will be able to help you find out more.
Pain relief afterwards
Good pain relief is important, and some people need more pain relief than others. It is much easier to relieve pain if it is dealt with before it gets bad. Pain relief can be increased, given more often, or given in different combinations.
Occasionally, pain is a warning sign that all is not well; therefore, you should always report it to your nurses and seek their advice and help.
Here are some ways of giving pain relief:
Pills, tablets or liquids to swallow
These are used for all types of pain. They take at least half an hour to work. You need to be able to eat, drink and not feel sick, for these drugs to work.
Injections
These are often needed and may be intravenous (through your cannula into a vein for a quicker effect) or intramuscular (into your leg or buttock muscle using a needle, taking about 20 minutes to work).
Suppositories
These waxy pellets are put in your rectum (back passage). The pellet dissolves and the drug passes into the body. They are useful if you cannot swallow or if you might vomit.
Patient-controlled analgesia (PCA)
A machine allows you to control your pain relief yourself. The medicine enters your body through your cannula. If you would like more information, ask for a leaflet on PCA.
Local anaesthetics and regional blocks
These types of anaesthesia can be very useful for relieving pain after surgery. More details can be found in the leaflet Epidural pain relief after surgery (www.rcoa.ac.uk/patientinfo
Local and regional anaesthetics
If you are having a local or regional anaesthetic:
- your anaesthetist will ask you to keep quite still while the injections are given. You may notice a warm tingling feeling as the anaesthetic begins to take effect
- your operation will only go ahead when you and your anaesthetist are sure that the area is numb
- you will remain alert and aware of your surroundings, unless you are having sedation. A screen shields the operating site, so you will not see the operation unless you want to
- if you are having sedation, you will be sleepy and relaxed. However, you may be aware of events around you
- for regional anaesthetics, your anaesthetist is always near to you and you can speak to him or her whenever you want to. For local anaesthetics, other theatre staff may be looking after you.
General anaesthetics
There are two ways of starting a general anaesthetic:
- anaesthetic drugs may be injected into a vein through the cannula. This is generally used for adults
- you can breathe anaesthetic gases and oxygen through a mask, which you may hold if you prefer.
Once you are unconscious, an anaesthetist stays with you at all times and continues to give you drugs to keep you anaesthetised.
The Recovery room: After the operation, you will usually be taken to the recovery room. Recovery staff will make sure you are as comfortable and free of nausea as possible. When they are satisfied that you have recovered safely from your anaesthetic you will be taken back to the ward.
Before coming to hospital
- If you smoke, giving up for several weeks before the operation will reduce the risk of breathing problems during your anaesthetic, making your anaesthetic safer.
- If you are very overweight, reducing your weight will reduce many of the risks of having an anaesthetic.
- If you have loose teeth or crowns, treatment from your dentist may reduce the risk of damage to your teeth during the anaesthetic.
- If you have a long-standing medical problem such as diabetes, asthma or bronchitis, thyroid problems, heart problems or high blood pressure, you should ask your GP if you need a check-up.
On the day of your operation
Nothing to eat or drink – (‘nil by mouth’)
The hospital should give you clear instructions about eating and drinking. These instructions are important. If there is food or liquid in your stomach during your anaesthetic, it could come up into your throat and damage your lungs.
If you are a smoker, you should not smoke on the day of your operation.
If you are taking medicines: most medicines should be continued before an operation, but there are some important exceptions. You will need specific instructions from the pre-assessment team about your tablets.
If you feel unwell when you are due to come into hospital, please telephone the ward for advice.
Meeting your anaesthetist
Your anaesthetist will meet you before your operation. They will refer to the discussion you had in the pre-assessment clinic. They will discuss the anaesthetic you could have, including benefits, risks and your preferences. They will then:
- decide with you which anaesthetic would be best for you
- decide for you, if you would prefer that.
If there is a choice of anaesthetic, this will depend on:
- the operation you are having and your physical condition
- your preferences and the reasons for them
- the recommendation of the anaesthetist, based on experience
- the equipment, staff and resources at the hospital.
Pre-medication (a ‘pre-med’) is given before some anaesthetics. Pre-meds prepare your body for surgery – they may start off the pain relief, reduce acid in the stomach or help you relax. Some pre-meds make you more drowsy after the operation. If you think a pre-med would help you, please ask your anaesthetist.
A needle is used to start most anaesthetics in adults. If you are very worried about this, please talk to your anaesthetist.
Sedation. This is the use of small amounts of anaesthetic or similar drugs to produce a ‘sleep like’ state. If you are having a local or regional anaesthetic, you will need to decide whether you would prefer to:
- be fully alert
- be relaxed and sleepy (sedation) but not unconscious
- have a general anaesthetic as well.
Nothing will happen to you until you understand and agree with what has been planned. You have the right to refuse if you do not want the treatment suggested or if you want more information or more time to decide.
When you are called for your operation
- A member of staff will go with you to the theatre.
- You can wear your glasses, hearing aids and dentures until you are in the anaesthetic room. You may be able to keep them on if you are having a local or regional anaesthetic.
- Jewellery and/or any decorative piercing should ideally be removed.
- If you cannot remove it, the nurses will cover it with tape to prevent damage to it or to your skin.
- If you are having a local or regional anaesthetic, you can take your own electronic device, with headphones to listen to music.
- You may walk to theatre, accompanied by a member of staff, or you may go in a wheelchair or on a bed or trolley. If you are walking, you can wear your own dressing gown and slippers.
- Final checks will be done as you arrive in the operating department, before the anaesthetic starts. You will be asked to confirm your name, the operation you are having, whether left or right side (if applicable), when you last ate or drank and your allergies. These routine checks are normal in all hospitals.
Starting the anaesthetic
Your anaesthetic may start in the anaesthetic room or in the operating theatre. Your anaesthetist will be working with a trained assistant. The anaesthetist or the assistant will attach machines that measure your heart rate, blood pressure and oxygen levels.
Almost all anaesthetics, including some kinds of local anaesthetic, start with a needle being used to put a cannula (thin plastic tube) into a vein in the back of your hand or arm. If needles worry you, please tell your anaesthetist. A needle cannot usually be avoided, but there are things he/she can do to help.
Due to individual variation, it may be more difficult to insert a cannula in some patients. Factors like BMI (body mass index), environmental temperature and prolonged fasting/starvation prior to surgery might make the insertion of this needle more challenging. It is rare to start the anaesthetic without this cannula in place. Rarely an ultrasound machine may be needed to assist insertion. An amount of bruising and discomfort may be experienced at the insertion site after the removal of the cannula. The level of bruising may vary based on certain medications and the indiviual’s tendency to bruise. Firm pressure at the site, after removal of the cannula, may reduce this. Very thin/fragile skin tends to bruise more readily. This bruising should resolve after a few days.
Questions you may like to ask your anaesthetist
- Who will give my anaesthetic?
- Do I have to have a general anaesthetic?
- What type of anaesthetic do you recommend?
- Have you often used this type of anaesthetic?
- Will I be unconscious and completely unaware during this kind of anaesthetic?
- What are the risks of this type of anaesthetic?
- Do I have any special risks?
- How will I feel afterwards?
Other useful resources to get you prepared for surgery can be found on this website below
https://www.rcoa.ac.uk/patient-information/preparing-surgery-fitter-better-sooner