The leaflet is detailed below, or you can download the 'Going home with an Indwelling Urethral Catheter' leaflet in PDF.
You are being discharged home with an indwelling urethral catheter. It should have been explained to you already why you need to have an indwelling urethral catheter, if not, please ask your health professional to explain this to you.
This leaflet is intended to give you information on how to look after your catheter and drainage system at home.
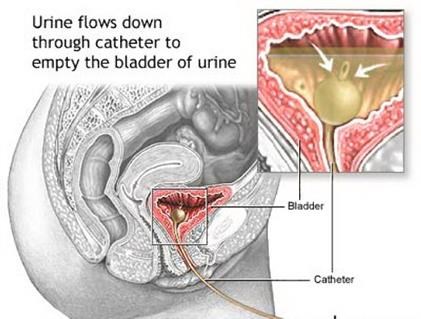
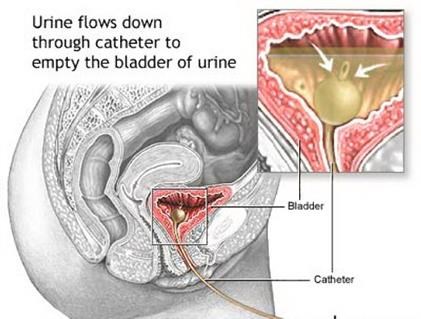
What is an Indwelling urethral catheter?
It is a hollow, flexible tube which drains urine from your bladder. A small balloon in your bladder, filled with water, stops the catheter from falling out.
Your catheter may be short term or long- term depending on your medical condition. This will be discussed with you by your health professional.
Indwelling urethral catheters and drainage bags
The urine will drain out through the catheter and into a drainage bag attached at the end. There are two types of drainage bag, a leg bag and a bed bag. You generally wear a leg bag during the day and at night you connect this to a larger bed bag.
During the day- Leg bags are worn under your clothing during the day. You will need to empty the urine out into the toilet every few hours via the tap at the bottom of the bag. Leg Bags are worn on your thigh, under your clothing, making them discreet to wear. They are held securely to your leg with either Velcro straps or a cotton sleeve.
Leg bags are available in three different sizes, 350mls, 500mls, and 750mls and with varying tube lengths. Your nurse will be able to advise you on the products available and which may be the best one for you.
During the night - At night, a larger drainage bag (bed bag) can be used to drain the urine when you are asleep. The bed bag is connected to the end of the leg bag, leaving the leg bag tap open to allow drainage. A bed bag needs to be supported off the floor or bed by hanging it on a stand.
It is advisable that you loosen the Velcro straps of the leg bag or remove the cotton sleeve at night.
Changing the drainage bags?
It is recommended that you change your leg bag every 5-7 days. However, if the bag gets damaged or becomes uncomfortable you may change it sooner.
To change your leg bag first wash your hands, then remove a new bag from its packaging. Empty the urine out of your existing leg bag then gently remove the bag from the end of the catheter and put it into a plastic bag for disposal. Remove the dust cap from the end of the new leg bag and insert the bag into the end of the catheter making sure it is pushed up as far as it will go.
When discarding your old leg bag, make sure it is empty, place it in a plastic bag in your household waste bin and wash your hands.
It is recommended that you use a non-drainable bed bag as this is emptied and discarded (as above) every morning and reduces the risk of infection.
Indwelling catheters with catheter valves
An alternative to drainage bags is a catheter valve. This is a simple tap that is attached to the end of the catheter and every 3-4 hours it is recommended that you open the valve and let the urine drain out of your bladder into the toilet.
Catheter valves are small and discreet and are supported either by tucking them into your underwear or wearing a special catheter leg strap around the top of your thigh. It is recommended that catheter valves are changed every 5-7 days. Your health professional will show you how to do this before you go home.
Not everyone is suitable for a catheter valve, and they should only be used after discussion and on the advice of your healthcare professional.
Personal hygiene
Personal hygiene is very important when you are living with an indwelling urethral catheter to help prevent infection. The following points are important to remember.
- Always wash your hands before and after emptying your drainage bag or opening your catheter valve.
- Try to have a bath or shower every day. Always empty your drainage bag first. If you are using catheter straps on your leg bag you may wish to have a pair just for use in the bath and shower.
- Never apply creams or talcum powder as they may cause “clogging” around the catheter entry site and may increase your risk of infection.
- Change your underwear daily.
- After having your bowels open always wipe your bottom from front to back. Wet wipes are useful and can be used to clean after having your bowels open.
Should I be drinking and eating anything different?
It is very important that you drink lots of fluid when you have an indwelling urethral catheter in place. Try to drink at least 2 litres (about 8 glasses) of fluid a day. This helps to keep the urine dilute and helps to prevent infection. Try to avoid caffeinated drinks (e.g. tea/coffee), fizzy and sugary drinks and alcohol.
You should continue to eat a normal, healthy balanced diet to avoid getting constipated. Constipation could affect how your catheter drains. Try to include plenty of fresh fruit, vegetables and whole grains to provide sufficient fibre. If you think you may be constipated you GP may be able to prescribe medication to help.
What about sex?
You can still have sex with a catheter in place if you follow the following steps.
- Tape the catheter onto your abdomen out of the way.
- Both partners should wash their genitals before and after intercourse.
- It may help using a lubricant, like KY jelly, YESWB or YESOB.
You must never remove your catheter unless you have been taught to do so.
If you have any problems or questions do not hesitate to discuss this with your health care
Can I travel with a Catheter?
Having a catheter should not stop or limit your ability to travel. You may connect a larger drainage bag (night bag) to your leg bag, if you desire however a leg bag should be sufficient for travel as long as it is emptied as recommended. If you intend to fly, then try to avoid alcohol as altitude dehydrates the body. Be sure to take spare catheters and other supplies with you on holidays or long journeys.
What problems can occur with a catheter?
When you first have your catheter inserted you may experience some or none of the following:
- A feeling you need to pass urine. This may be caused by irritation to the bladder or urethra and should settle after a few days.
- A bladder spasm or cramp from time to time. Again, this usually settles after a few days and is nothing to worry about. Walking around whilst you have a spasm can help or alternatively, take a mild painkiller.
- Urine leaking around the catheter. This may happen when you have a bladder spasm. As long as urine is draining into the bag or out through the valve this is not an emergency. However, if it continues you should inform the health professional who is managing your care.
If you find the urine has stopped draining into the bag or no urine comes out when you open the catheter valve, then you need to check the following:
- Make sure there are no kinks in the catheter or tubing of the drainage bag.
- Check the drainage bag is below the level of your bladder.
- Check the drainage bag is connected the right way up Make sure you are drinking enough fluids
- Are you constipated?
Could I get a urine infection with an indwelling urethral catheter?
Yes, it is a risk. Having a catheter can increase your risk of getting a urine infection. You can help prevent this happening by making sure you drink plenty of clear fluids, such as water or diluted juice, avoid constipation, ensure you maintain a good level of hygiene and never let anyone else empty or change your catheter or drainage bag unless they have been trained to do so.
Symptoms of a urine infection include dark, cloudy, offensive smelling urine, increased body temperature and aching and pain.
When do I ask for help or advice?
You will need to contact someone for advice if you experience any of the symptoms described in this below
If you have prolonged pain which has not been relieved with painkillers or movement
- If your urine has not drained after 2-3 hours
- If there is blood in your urine which does not clear after drinking extra fluids
- If you think you have a urine infection
- If urine keeps leaking around your catheter
Your GP or local Walk-in centre can advise, if this is closer to home. Please remember to take you catheter passport along.
The following are contact number at the Liverpool Women’s Hospital: -
Non urgent answer phone service - Urogynaecology Nurse practitioners 0151 702 4321 Mon – Friday 8.30-4.30
Maternity Assessment Unit (MAU) i0151 702 4413
Main hospital Number 0151 708 9988
Call 111 for advice or attend the Gynecology Emergency Department (GED) at Liverpool Women’s or your nearest Accident and emergency Service if your concerns are urgent.
Trial Without Catheter (TWOC)
You may need to attend the TWOC clinic to have your catheter removed. This clinic is held in Gynae Outpatients Department (GOPD).
How long will I be at the clinic?
You may be at the clinic for 2-4 hours but could be longer depending on your hydration.
If you have a catheter valve, please do not open your valve for two hours prior to attending the clinic we also advise you drink 500mls water, slowly over 1-2 hours before your appointment. This will allow your bladder to fill before you arrive in the clinic.
What will happen at the clinic?
Once your catheter is removed, we will assess how well you can pass urine.
If you have had a catheter valve and your bladder is full, then we will assess how you can empty your bladder immediately. If you have had a catheter bag, then you will need to fill your bladder. We have a waiting area where you will have access to drinking water or alternatively you can bring in your own drinks.
What if I can’t pass urine?
If you can’t pass urine the nurse will assess how full your bladder is. If your bladder hasn’t filled enough, you will be encouraged to drink a little more and wait a bit longer.
If your bladder is very full, then you will be taught how to self-catheterise (insert a catheter into your bladder yourself). If you are unable to do this, then the nurse will reinsert an indwelling catheter with a catheter valve.
Going Home?
The nurse will inform you of future follow up appointments and provide you with contact phone numbers.
Contact phone numbers: -
Non urgent answer phone service - Urogynaecology Nurse practitioners 0151 702 4321 Mon – Friday 8.30-4.30
Maternity Assessment Unit 0151 702 4413
Main hospital Number 0151 708 9988