Advice and exercise following a Caesarean section:
A Caesarean section is a major operation, which involves an incision (cut) through the tummy muscles and womb. It may take up to 6-12 weeks to recover, for some women this may be longer, and it is important to allow yourself time to rest and recover.
It is common to experience pain/discomfort for the first few weeks when moving, getting in/out of bed or carrying out activities that cause strain on your tummy. Having anaesthetic can also cause you to feel more tired than usual and may cause sickness. However, it is important to start moving as soon as possible as it will help with your circulation, breathing and prevent your muscles and joints from getting too sore and stiff. You should be given pain relief after your caesarean to help you do this.
Please view our link with further information: Caesarean section
How to exercise the pelvic floor muscles:
Pelvic floor exercises should include long squeezes as well as short, quick squeezes, making sure you let go/relax the muscle between each squeeze. Aim to complete both long and short squeezes 3 times a day. Start by sitting in a comfortable position, feet flat on the floor or lying on your back or side with your knees bent. Imagine that you are trying to stop yourself passing wind. You want to feel the muscle around your back passage tightening and drawing upwards and forwards towards your tummy button. At the same time, if you can, think about trying to stop yourself passing urine ‘wee’. Try not to clench/squeeze the buttock muscles or hold your breath. Don’t try to stop and start the flow of urine whilst on the toilet – this can interfere with normal bladder function.
- Long Squeezes: To begin, aim to hold the squeeze for 5 seconds. Let go. Relax for a few seconds. Repeat 5 times. As the muscle gets stronger, aim to hold for up to 10 seconds and up to 10 repetitions.
- Short, quick squeezes: Quickly squeeze the pelvic floor and then let go immediately. To begin with, aim to repeat 5 short squeezes. Make sure you relax the pelvic floor between each squeeze. As the muscle gets stronger, aim for 10 short squeezes.
Going home and returning to exercise:
You will need to rest at home, but it is important that you carry on with pelvic floor exercises, increasing the repetitions as you get stronger. Whilst your abdominal scar will heal quickly, it is important that you exercise at a steady rate to allow your deeper muscles to recover. Please see the leaflet ‘Improving your pelvic health and fitness after pregnancy’ for more exercises.
Walking for a short distance every day will help to improve your strength and fitness, and you should try to increase the pace and distance achieved as you feel able. For more information on returning to exercise visit: www.thepogp.co.uk and their information booklet ‘Fit for the Future’.
Try to avoid any heavy lifting until you are 6 weeks post-natal. Avoid any activities that causes strain for the first few weeks e.g. vacuuming, prolonged standing, carrying toddlers etc.
When to return back to exercise:
Generally, you can start easing back into exercise six to eight weeks after having a c-section. It’s important to note that you may not have the same c-section recovery experiences and timelines as other people you know who have had caesarean deliveries, so it’s key to listen to your own body and your healthcare provider's recommendations.
There are some very light exercises and movements you can do prior to your six-week postnatal check including light pelvic floor exercises (see above), gently tightening your abdominal muscles in a sitting or lying position to activate them.
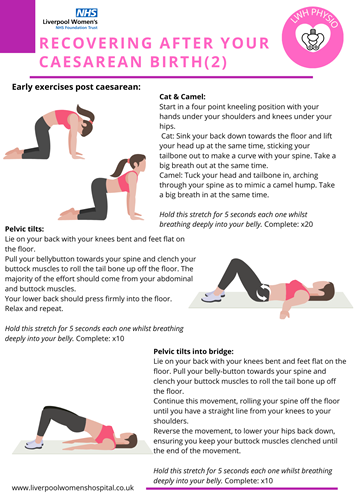
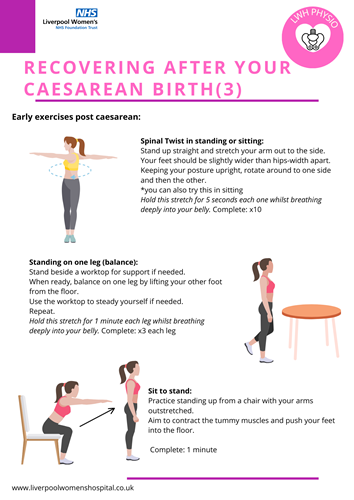
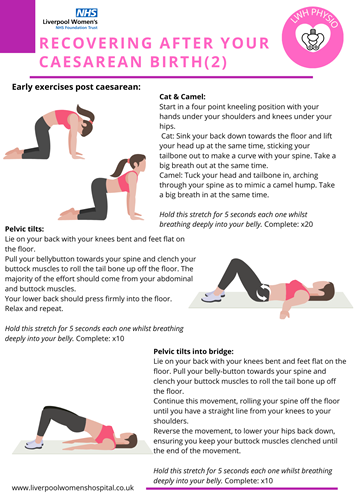
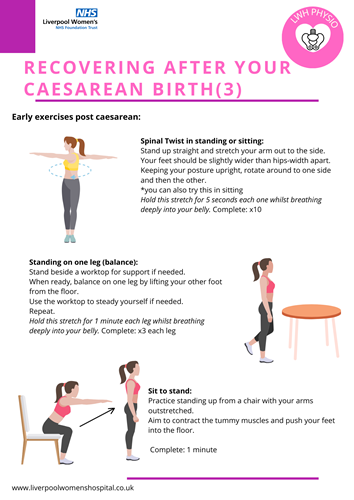
Please view our early rehab exercises